Paperwork
COBRA Paperwork Return Deadline
Understanding COBRA Paperwork Return Deadline
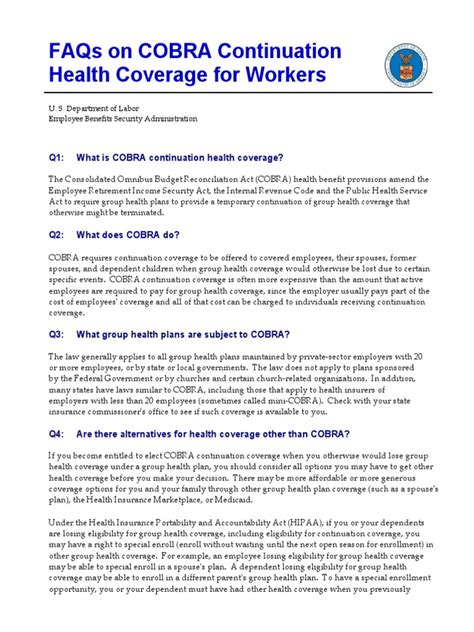
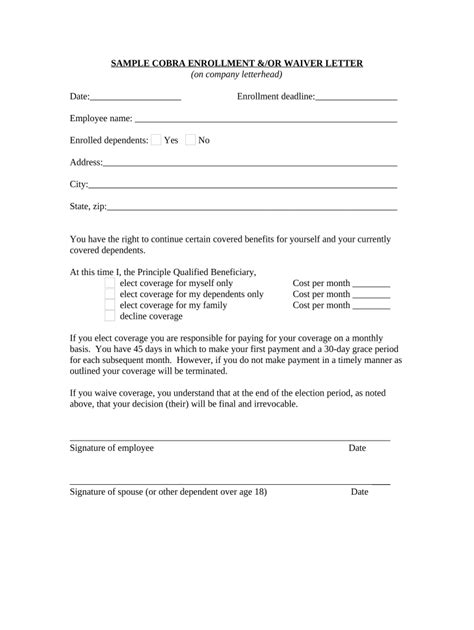
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that allows certain former employees, spouses, and dependents to temporarily continue their health coverage at their own expense. One of the critical aspects of COBRA administration is the timely return of paperwork, which includes the election form and payment of premiums. In this article, we will delve into the specifics of the COBRA paperwork return deadline, its implications, and the steps involved in the process.
What is the COBRA Paperwork Return Deadline?
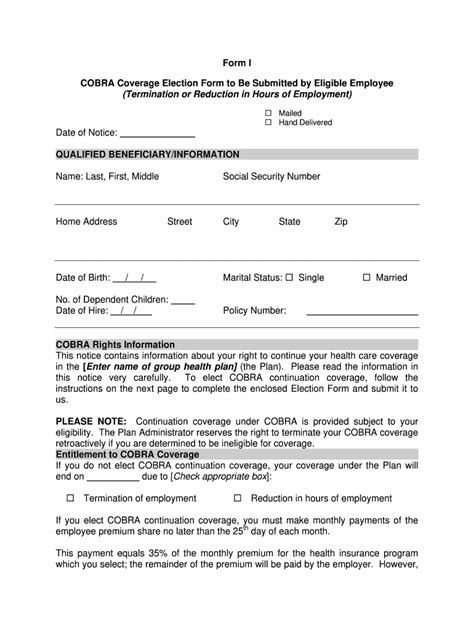
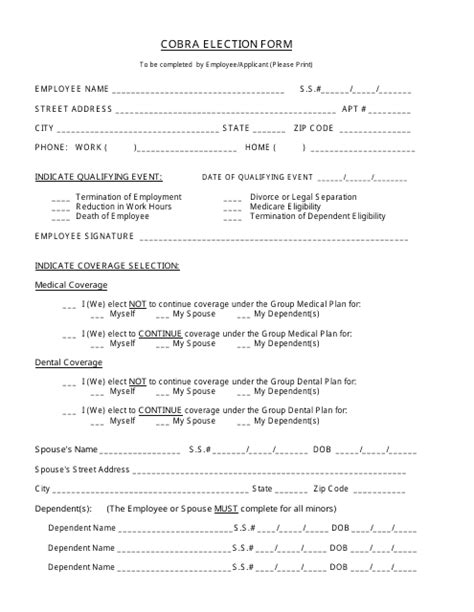
The COBRA paperwork return deadline refers to the timeframe within which the qualified beneficiary must return the election form to the plan administrator. Generally, the qualified beneficiary has 60 days from the date they receive the election notice to decide whether to elect COBRA coverage. This period is crucial as it allows the beneficiary sufficient time to consider their options and make an informed decision regarding their health insurance.
Key Steps in the COBRA Election Process
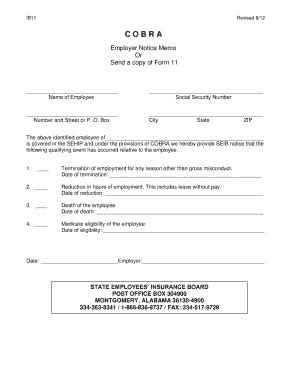
The COBRA election process involves several key steps: * The plan administrator must provide the qualified beneficiary with an election notice within 14 days after the qualifying event (e.g., termination of employment, divorce, or death of the covered employee). * The qualified beneficiary then has 60 days from the date they receive the election notice to return the completed election form to the plan administrator. * Upon receipt of the election form, the plan administrator must provide the qualified beneficiary with a confirmation of their election, including the terms of the coverage and the premium payment details. * The qualified beneficiary is responsible for making timely premium payments to maintain COBRA coverage.
Importance of Meeting the Deadline

Meeting the COBRA paperwork return deadline is essential to avoid loss of coverage. If the qualified beneficiary fails to return the election form within the 60-day window, they will forfeit their right to COBRA coverage. Furthermore, if the premium payment is not made on time, the plan administrator may terminate the COBRA coverage.
📝 Note: It is crucial for qualified beneficiaries to carefully review the election notice and understand the deadline for returning the paperwork to avoid any potential gaps in health coverage.
Consequences of Missing the Deadline

Missing the COBRA paperwork return deadline can have significant consequences, including: * Loss of COBRA coverage * Gaps in health insurance * Increased costs due to medical expenses or penalties for lack of coverage * Potential loss of eligibility for other health insurance options
Best Practices for Plan Administrators

To ensure compliance with COBRA regulations, plan administrators should: * Provide clear and timely election notices to qualified beneficiaries * Establish a system for tracking and responding to election forms and premium payments * Maintain accurate records of COBRA coverage and premium payments * Communicate effectively with qualified beneficiaries regarding their rights and responsibilities under COBRA
Conclusion
In summary, the COBRA paperwork return deadline is a critical aspect of the COBRA administration process. Qualified beneficiaries must return the election form within 60 days of receiving the election notice to maintain their health coverage. Plan administrators must provide timely and clear election notices, track and respond to election forms and premium payments, and maintain accurate records to ensure compliance with COBRA regulations. By understanding the COBRA paperwork return deadline and following best practices, qualified beneficiaries can make informed decisions about their health insurance, and plan administrators can ensure compliance with federal regulations.
What is the timeframe for returning the COBRA election form?
+
The qualified beneficiary has 60 days from the date they receive the election notice to return the completed election form to the plan administrator.
What happens if the qualified beneficiary misses the deadline for returning the election form?
+
If the qualified beneficiary fails to return the election form within the 60-day window, they will forfeit their right to COBRA coverage.
What are the consequences of missing the deadline for premium payment?
+
If the premium payment is not made on time, the plan administrator may terminate the COBRA coverage, resulting in gaps in health insurance and potential increased costs due to medical expenses or penalties.