5 Medicaid Paperwork Tips
Introduction to Medicaid Paperwork
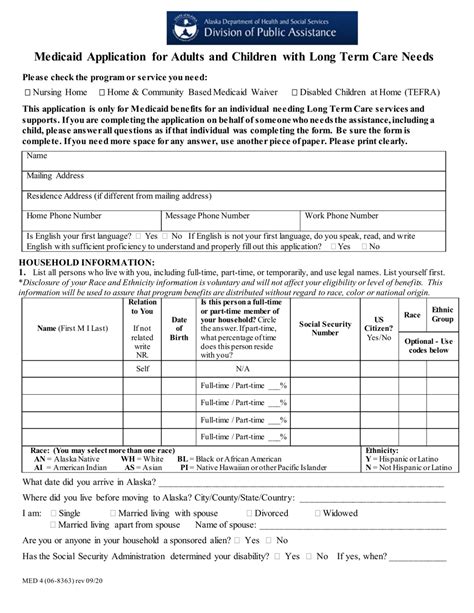
Medicaid is a federal and state program that provides health coverage to millions of Americans, including low-income individuals, families, and children, as well as people with disabilities and elderly individuals who require nursing home care. The process of applying for and managing Medicaid benefits often involves a significant amount of paperwork, which can be overwhelming for many applicants and beneficiaries. Understanding the key aspects of Medicaid paperwork and how to navigate the system efficiently is crucial for ensuring that eligible individuals receive the benefits they need.
Understanding Medicaid Eligibility

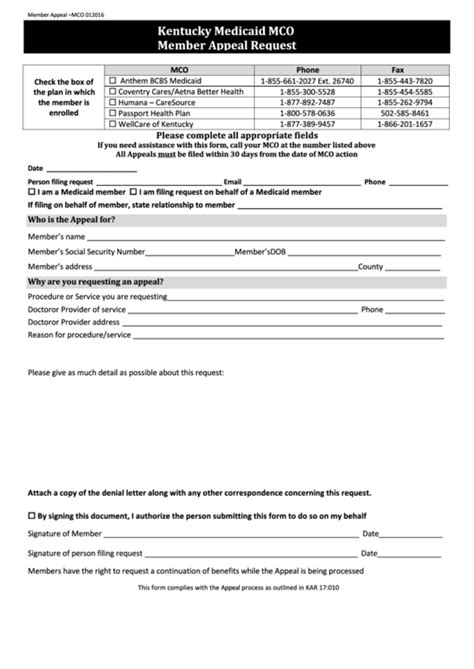
Before delving into the specifics of Medicaid paperwork, it’s essential to understand the eligibility criteria for the program. Eligibility varies from state to state, but it generally includes factors such as income, family size, disability status, and other requirements. Income limits and family size are particularly important, as they determine whether an individual or family qualifies for Medicaid. Additionally, some states have expanded their Medicaid programs to cover more individuals, including childless adults with incomes up to a certain percentage of the federal poverty level.
5 Tips for Managing Medicaid Paperwork
Given the complexity and volume of paperwork associated with Medicaid, here are five tips to help individuals and families manage the process more effectively:
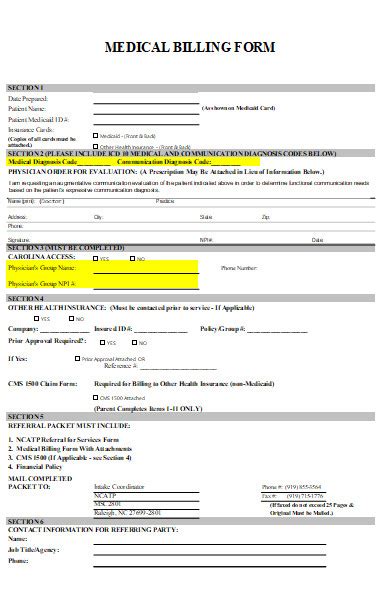
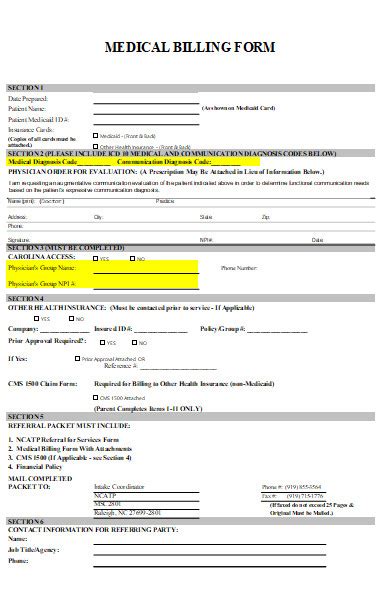
- Keep Detailed Records: Maintaining detailed and organized records of all paperwork, including applications, renewals, and communications with Medicaid officials, is crucial. This can help in tracking the status of applications, ensuring that all required documents are submitted, and resolving any issues that may arise.
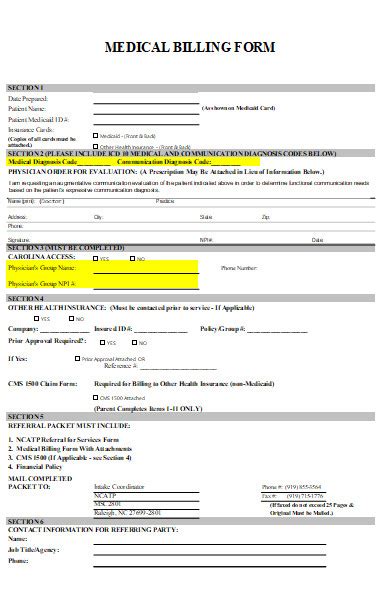
- Understand the Application Process: The Medicaid application process can vary significantly from one state to another. It’s vital to understand the specific requirements and procedures in your state, including how to apply, what documents are needed, and how long the process typically takes.
- Seek Assistance When Needed: Navigating Medicaid paperwork can be challenging, especially for those who are not familiar with the system or who have limited experience with bureaucratic processes. Seeking assistance from social workers, patient advocates, or non-profit organizations that specialize in healthcare access can provide invaluable guidance and support.
- Stay Informed About Eligibility and Benefits: Medicaid eligibility and benefits can change over time due to updates in federal or state policies, changes in personal circumstances, or other factors. Staying informed about these changes and how they may affect your benefits is essential for ensuring continuous coverage.
- Review and Update Information Regularly: Regularly reviewing and updating your Medicaid information can help prevent gaps in coverage and ensure that you continue to receive the benefits you are eligible for. This includes reporting changes in income, family size, or other eligibility factors to your state’s Medicaid agency.
Common Challenges with Medicaid Paperwork
Despite the best efforts to manage Medicaid paperwork efficiently, individuals and families may encounter several challenges. These can include delays in processing applications, difficulty in obtaining required documents, and confusion over eligibility criteria. Additionally, language barriers and lack of access to technology can further complicate the process for some applicants and beneficiaries.
Role of Technology in Simplifying Medicaid Paperwork
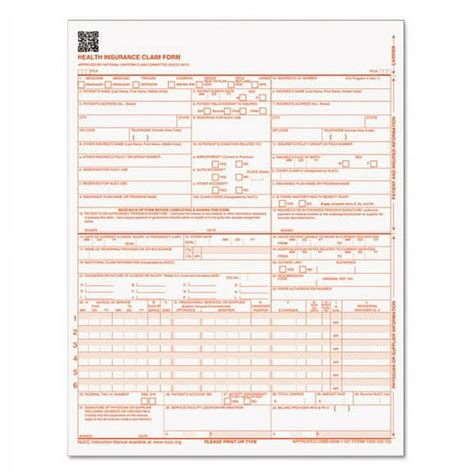
Technology has the potential to significantly simplify the Medicaid paperwork process. Many states offer online application portals where individuals can apply for Medicaid, upload required documents, and track the status of their applications. Moreover, digital record-keeping systems can help in maintaining accurate and up-to-date records, reducing the risk of errors and lost documents.
| State | Medicaid Expansion Status | Income Limit for Eligibility |
|---|---|---|
| California | Expanded | Up to 138% of FPL |
| New York | Expanded | Up to 138% of FPL |
| Texas | Not Expanded | Varies by Category |
📝 Note: The information provided in the table is a simplified example and may not reflect the current Medicaid expansion status or income limits for eligibility in each state. It's essential to check with your state's Medicaid agency for the most accurate and up-to-date information.
In summary, managing Medicaid paperwork requires a thorough understanding of the program’s eligibility criteria, application process, and the importance of maintaining detailed records. By following the tips outlined above and leveraging technology to simplify the process, individuals and families can more effectively navigate the system and ensure they receive the Medicaid benefits they are eligible for. This knowledge is critical for accessing necessary healthcare services and maintaining overall well-being. Ultimately, understanding and efficiently managing Medicaid paperwork is a key component of ensuring that eligible individuals and families receive the healthcare coverage they need.
What is the primary purpose of Medicaid?
+
The primary purpose of Medicaid is to provide health coverage to low-income individuals and families, including children, pregnant women, elderly individuals, and people with disabilities.
How do I apply for Medicaid?

+
You can apply for Medicaid through your state’s Medicaid agency, either online, by phone, or in person. The application process typically involves providing personal and financial information to determine eligibility.
What documents are required for Medicaid eligibility?

+
Required documents for Medicaid eligibility may include proof of income, citizenship or immigration status, social security number, and identification. The specific documents needed can vary by state and individual circumstances.