Fill Out Cobra Paperwork Easily
Understanding COBRA: A Comprehensive Guide
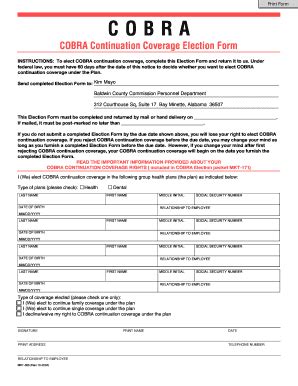
The Consolidated Omnibus Budget Reconciliation Act, commonly referred to as COBRA, is a federal law that allows certain employees and their families to continue their health insurance coverage after a job loss or other qualifying event. Navigating the process of filling out COBRA paperwork can seem daunting, but with the right guidance, it can be a straightforward and manageable task. In this article, we will delve into the details of COBRA, its eligibility criteria, and provide step-by-step instructions on how to fill out the necessary paperwork.
Eligibility Criteria for COBRA

To be eligible for COBRA, individuals must meet specific criteria. These include: - Being covered under a group health plan sponsored by an employer with 20 or more employees. - Experiencing a qualifying event such as job loss, divorce, death of the covered employee, or a child losing dependent status. - Not being eligible for other group health coverage, except in certain circumstances. - Not having been terminated from employment due to gross misconduct.
Understanding these criteria is crucial before proceeding with the COBRA application process.
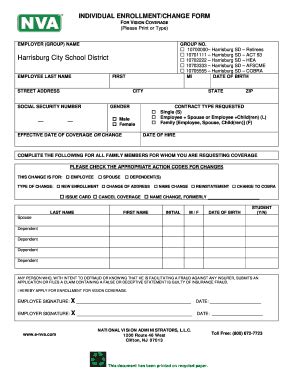
Steps to Fill Out COBRA Paperwork

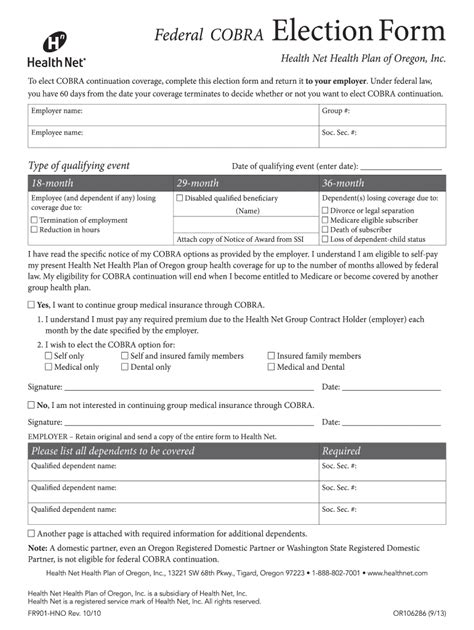
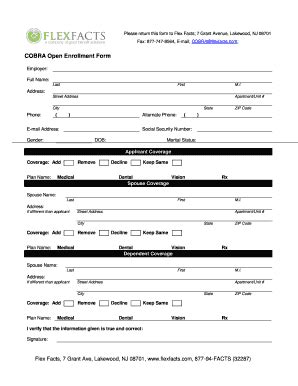
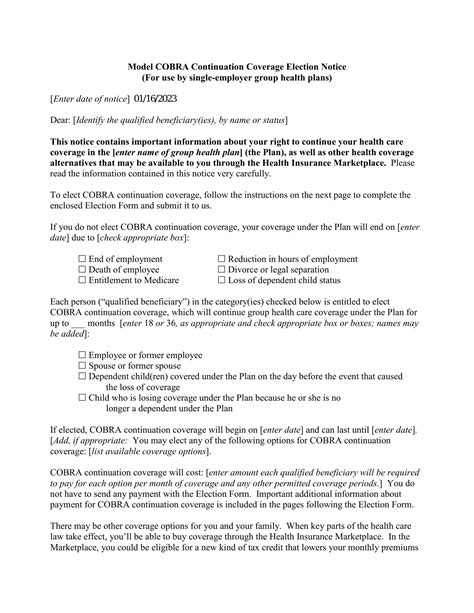
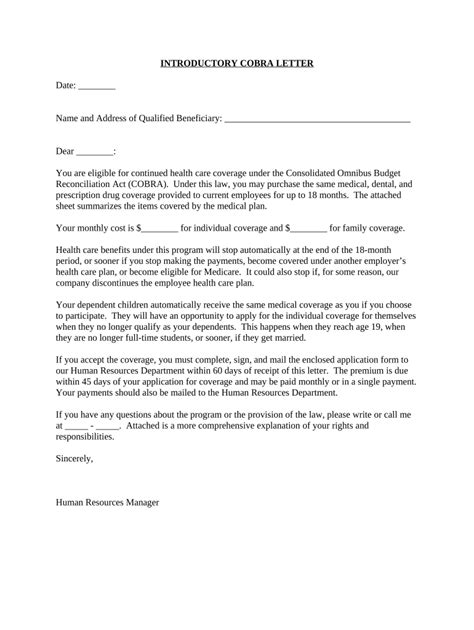
Filling out COBRA paperwork involves several steps, each designed to ensure that applicants provide all necessary information to process their request. Here’s a breakdown of the process: - Step 1: Receive the Election Notice: After a qualifying event, the employer or plan administrator must provide an election notice to the qualified beneficiaries. This notice explains the right to elect COBRA continuation coverage and how to make an election. - Step 2: Review the Notice Carefully: It is essential to review the election notice and any accompanying documentation carefully. This includes understanding the coverage options, the cost, and the deadlines for electing COBRA. - Step 3: Complete the Election Form: If the decision is made to elect COBRA, the next step is to complete the election form. This form is usually provided with the election notice and must be returned to the plan administrator by the specified deadline. - Step 4: Submit the Form: The completed election form should be submitted according to the instructions provided. This may involve mailing the form to a specified address or submitting it electronically, depending on the plan’s requirements. - Step 5: Make Premium Payments: Once COBRA coverage is elected, the individual is responsible for making timely premium payments. Failure to make payments can result in termination of coverage.
Important Considerations
When filling out COBRA paperwork, there are several important considerations to keep in mind: - Deadline for Election: There is a 60-day deadline from the date of the election notice or the date of the qualifying event, whichever is later, to elect COBRA coverage. - Premium Costs: COBRA premiums can be expensive, as they include the full cost of the coverage plus a 2% administration fee. - Duration of Coverage: COBRA coverage typically lasts for 18 months, although it can be extended in certain circumstances.
| Qualifying Event | Maximum Coverage Period |
|---|---|
| Employee termination or reduction of hours | 18 months |
| Death of the covered employee | 36 months |
| Divorce or legal separation | 36 months |
| Dependent child losing dependent status | 36 months |
📝 Note: It is crucial to carefully review all documentation and understand the terms and conditions of COBRA coverage before making a decision.
Alternatives to COBRA

While COBRA provides a valuable option for continuing health insurance coverage, it is not the only alternative. Other options may include: - Affordable Care Act (ACA) Marketplace Plans: These plans offer comprehensive coverage and may be more affordable than COBRA, especially for those who qualify for subsidies. - Spouse’s Plan: If a spouse has coverage through their employer, it may be possible to join their plan. - Short-Term Limited-Duration Insurance (STLDI): These plans provide temporary coverage and can be a more affordable option, although they typically offer less comprehensive coverage.
In conclusion, navigating the process of filling out COBRA paperwork requires a clear understanding of the eligibility criteria, the steps involved in the application process, and the alternatives available. By carefully considering these factors, individuals can make informed decisions about their health insurance coverage during times of transition.
What is the deadline for electing COBRA coverage?
+
The deadline for electing COBRA coverage is 60 days from the date of the election notice or the date of the qualifying event, whichever is later.
How long does COBRA coverage typically last?
+
COBRA coverage typically lasts for 18 months, although it can be extended in certain circumstances, such as the death of the covered employee, divorce, or a child losing dependent status, in which case it can last up to 36 months.
Are there alternatives to COBRA coverage?
+
Yes, alternatives to COBRA include Affordable Care Act (ACA) Marketplace Plans, a spouse’s employer-sponsored plan, and Short-Term Limited-Duration Insurance (STLDI). It’s essential to compare these options based on cost, coverage, and eligibility criteria.