Processing Cobra Paperwork Made Easy
Introduction to Cobra Paperwork
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that requires employers with 20 or more employees to offer continued health coverage to employees and their dependents after a qualifying event, such as job loss or divorce. Managing COBRA paperwork can be a daunting task for employers, but with the right guidance, it can be made easy. In this article, we will delve into the world of COBRA paperwork and provide you with a step-by-step guide on how to process it efficiently.
Understanding COBRA Qualifying Events

Before we dive into the paperwork, it’s essential to understand what constitutes a COBRA qualifying event. These events include: * Voluntary or involuntary termination of employment * Reduction in hours of employment * Divorce or legal separation * Death of the covered employee * Dependent child ceasing to be a dependent under the plan * Employee becoming entitled to Medicare It’s crucial to identify these events to determine when COBRA coverage should be offered.
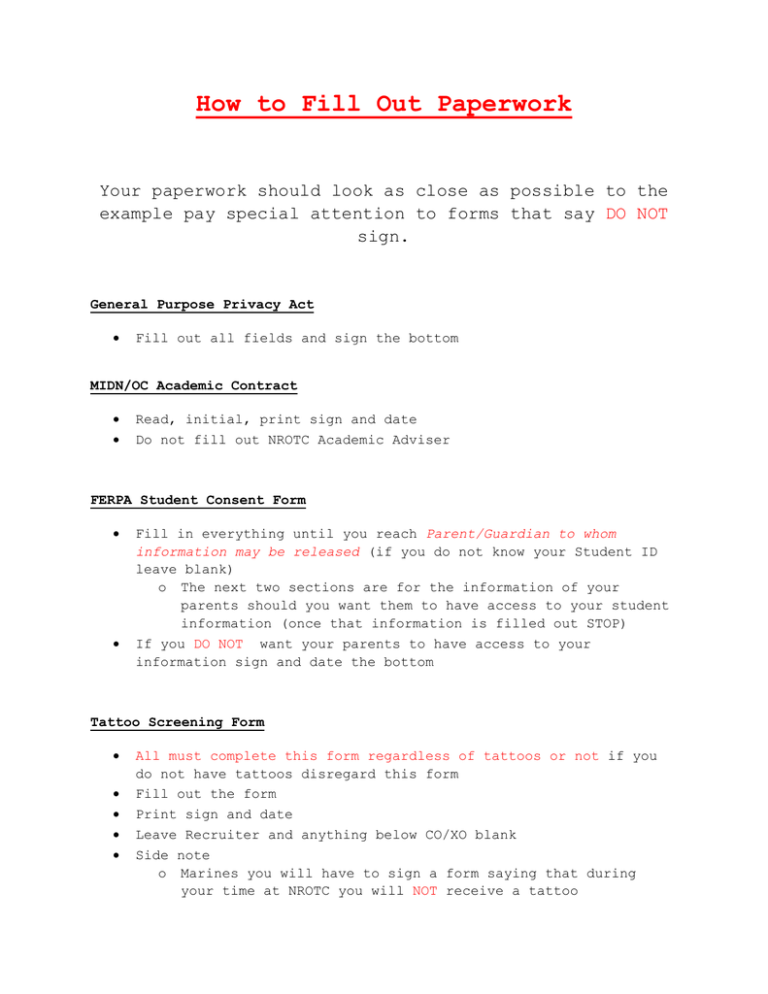
Step-by-Step Guide to Processing COBRA Paperwork
Processing COBRA paperwork involves several steps, which we will outline below: * Step 1: Notify the COBRA Administrator: The employer must notify the COBRA administrator within 30 days of a qualifying event. This can be done by completing a Notice of Qualifying Event form. * Step 2: Send the COBRA Election Notice: The COBRA administrator must send the COBRA election notice to the qualified beneficiary within 14 days of receiving the notice of qualifying event. This notice must include information about the COBRA coverage, premiums, and enrollment procedures. * Step 3: Collect Premium Payments: The qualified beneficiary must pay the premium for COBRA coverage within 45 days of electing coverage. The employer must collect these payments and remit them to the insurer. * Step 4: Maintain Records: The employer must maintain accurate records of all COBRA-related paperwork, including notices, election forms, and premium payments.
COBRA Paperwork Requirements
The following are the essential COBRA paperwork requirements:
| Document | Description |
|---|---|
| Notice of Qualifying Event | Notifies the COBRA administrator of a qualifying event |
| COBRA Election Notice | Notifies the qualified beneficiary of COBRA coverage and enrollment procedures |
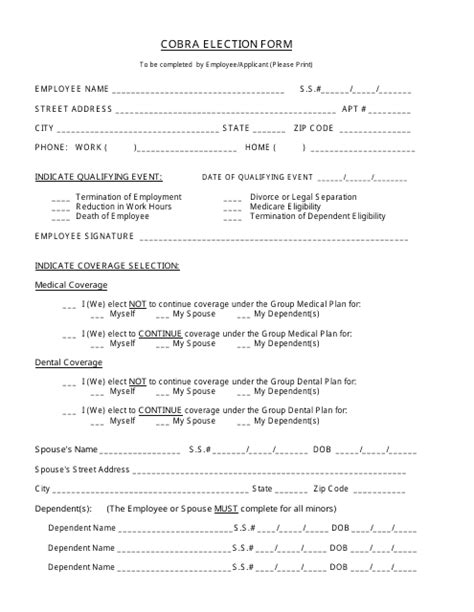
| COBRA Enrollment Form | Allows the qualified beneficiary to elect COBRA coverage |
| Premium Payment Form | Allows the qualified beneficiary to pay premiums for COBRA coverage |
Common COBRA Paperwork Mistakes to Avoid

To avoid common mistakes, employers should: * Ensure timely notification of qualifying events * Provide accurate and complete COBRA election notices * Collect and remit premium payments correctly * Maintain accurate records of all COBRA-related paperwork By avoiding these mistakes, employers can ensure compliance with COBRA regulations and avoid potential penalties.
📝 Note: Employers should consult with a COBRA expert or attorney to ensure compliance with all COBRA regulations and requirements.
In summary, processing COBRA paperwork requires attention to detail and a thorough understanding of the regulations. By following the steps outlined in this article and avoiding common mistakes, employers can ensure compliance and provide seamless COBRA coverage to their employees and dependents. The key takeaways from this article include understanding COBRA qualifying events, following the step-by-step guide to processing COBRA paperwork, and maintaining accurate records of all COBRA-related paperwork. With the right guidance and expertise, managing COBRA paperwork can be made easy, allowing employers to focus on their core business operations.
What is COBRA and how does it work?
+
COBRA is a federal law that requires employers with 20 or more employees to offer continued health coverage to employees and their dependents after a qualifying event. The employer must notify the COBRA administrator, who then sends the COBRA election notice to the qualified beneficiary. The qualified beneficiary can then elect COBRA coverage and pay premiums to maintain coverage.
What are the COBRA qualifying events?

+
The COBRA qualifying events include voluntary or involuntary termination of employment, reduction in hours of employment, divorce or legal separation, death of the covered employee, dependent child ceasing to be a dependent under the plan, and employee becoming entitled to Medicare.
How long do qualified beneficiaries have to elect COBRA coverage?

+
Qualified beneficiaries have 60 days to elect COBRA coverage from the date of the qualifying event or the date they receive the COBRA election notice, whichever is later.