5 Steps for COBRA Paperwork
Introduction to COBRA Paperwork
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that requires employers to offer continuation of health coverage to employees and their dependents in certain situations, such as when an employee loses their job or experiences a reduction in work hours. The COBRA paperwork process can be complex and time-consuming, but it’s essential to ensure compliance with the law. In this article, we’ll break down the 5 steps for COBRA paperwork and provide tips for a smooth and efficient process.
Step 1: Determine COBRA Eligibility
The first step in the COBRA paperwork process is to determine whether an individual is eligible for continuation coverage. To be eligible, an individual must have been covered under the employer’s health plan on the day before the qualifying event, such as a job loss or reduction in work hours. The qualifying event must also be one that is specified under COBRA, such as: * Voluntary or involuntary termination of employment * Reduction in work hours * Death of the covered employee * Divorce or legal separation * Dependent child ceasing to be a dependent under the plan It’s essential to review the employer’s health plan and COBRA policies to determine eligibility.
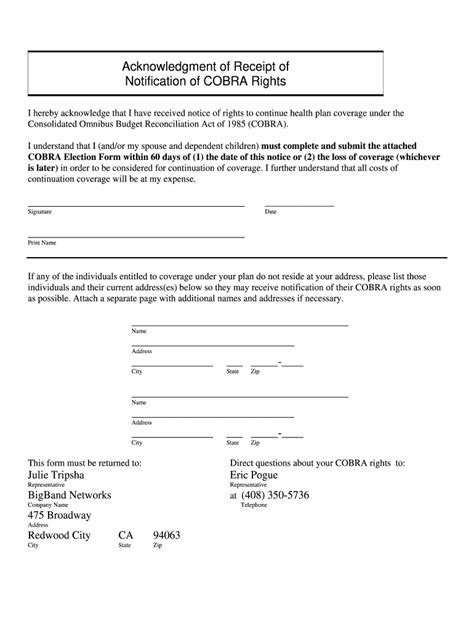
Step 2: Notify the Plan Administrator
Once an individual has been determined to be eligible for COBRA, the next step is to notify the plan administrator. The plan administrator is typically the employer or the insurance company that administers the health plan. The notification must be in writing and must include: * The individual’s name and address * The qualifying event that triggered COBRA eligibility * The date of the qualifying event * A request for COBRA continuation coverage The plan administrator must receive the notification within 60 days of the qualifying event.
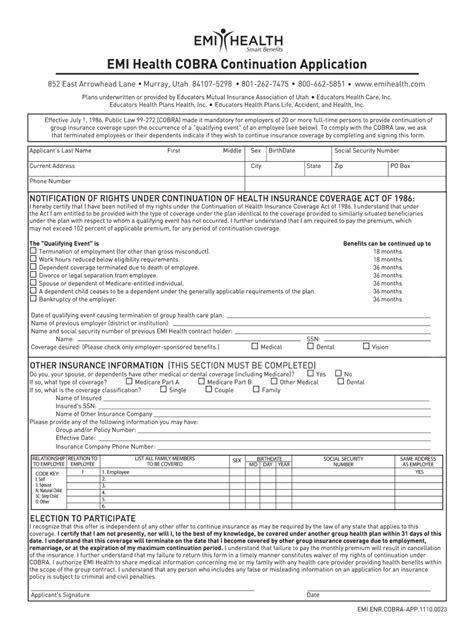
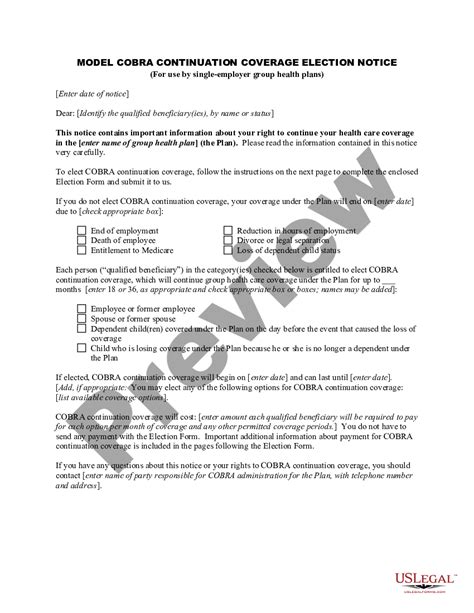
Step 3: Provide COBRA Election Notice
After receiving the notification, the plan administrator must provide the individual with a COBRA election notice. The election notice must include: * A description of the COBRA continuation coverage * The cost of the COBRA continuation coverage * The duration of the COBRA continuation coverage * Instructions for electing COBRA continuation coverage The individual must receive the election notice within 14 days of the plan administrator receiving the notification.
Step 4: Elect COBRA Continuation Coverage
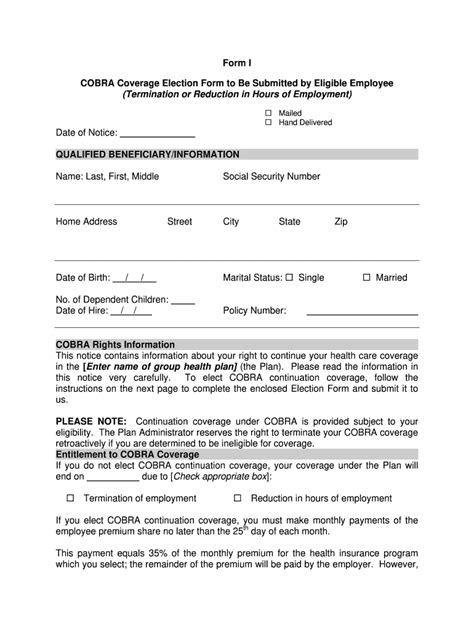
The individual must elect COBRA continuation coverage within 60 days of receiving the election notice. The election must be in writing and must include: * The individual’s name and address * A statement electing COBRA continuation coverage * The desired coverage start date The individual must also pay the first premium payment within 45 days of electing COBRA continuation coverage.
Step 5: Maintain COBRA Continuation Coverage
Once an individual has elected COBRA continuation coverage, they must maintain the coverage by paying premiums on time. The premiums must be paid within 30 days of the due date, and the individual must also notify the plan administrator of any changes in address or dependent status. COBRA continuation coverage typically lasts for 18 months, but it may be extended in certain situations, such as: * Disability: up to 29 months * Divorce or legal separation: up to 36 months * Dependent child ceasing to be a dependent: up to 36 months It’s essential to review the employer’s health plan and COBRA policies to determine the duration of COBRA continuation coverage.
💡 Note: It's crucial to keep accurate records of all COBRA paperwork, including notifications, election notices, and premium payments, to ensure compliance with the law and to avoid any potential disputes or penalties.
To summarize the key points, the 5 steps for COBRA paperwork include determining eligibility, notifying the plan administrator, providing a COBRA election notice, electing COBRA continuation coverage, and maintaining the coverage. By following these steps and maintaining accurate records, individuals can ensure a smooth and efficient COBRA paperwork process.
What is COBRA continuation coverage?
+
COBRA continuation coverage is a temporary extension of health coverage that is offered to individuals who have lost their job or experienced a reduction in work hours.
How long does COBRA continuation coverage last?

+
COBRA continuation coverage typically lasts for 18 months, but it may be extended in certain situations, such as disability, divorce or legal separation, or dependent child ceasing to be a dependent.
What are the qualifying events that trigger COBRA eligibility?
+
The qualifying events that trigger COBRA eligibility include voluntary or involuntary termination of employment, reduction in work hours, death of the covered employee, divorce or legal separation, and dependent child ceasing to be a dependent under the plan.