5 Medicaid Forms
Understanding Medicaid Forms: A Comprehensive Guide
Medicaid is a federal and state program that provides health coverage to eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. The application and enrollment process for Medicaid involves various forms that individuals must fill out to determine their eligibility and receive benefits. In this guide, we will explore five key Medicaid forms that play a crucial role in the application and enrollment process.
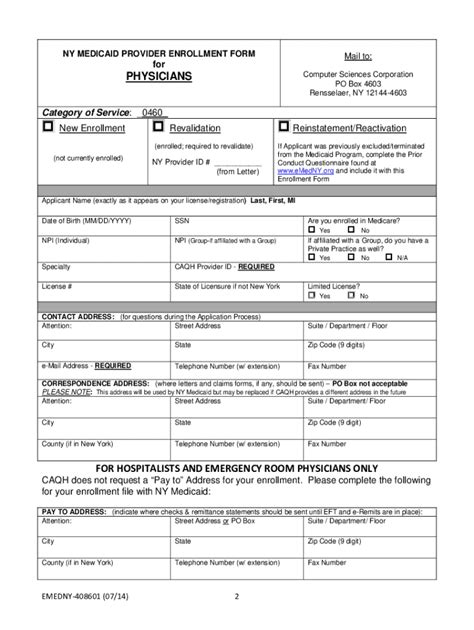
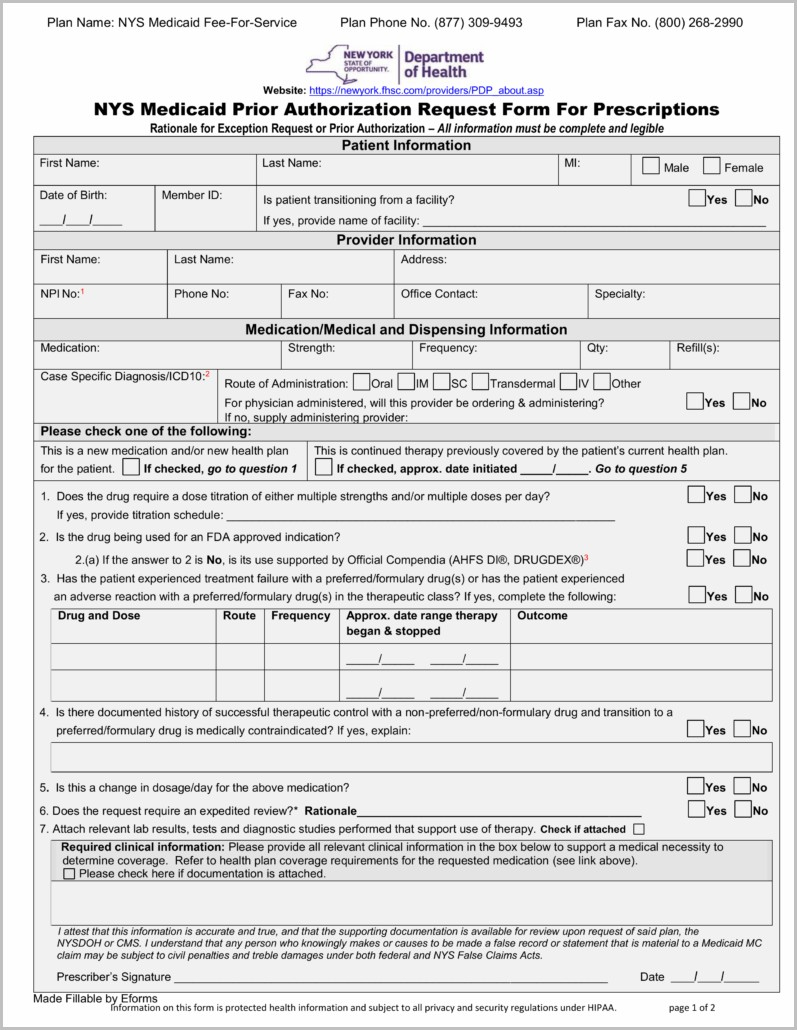
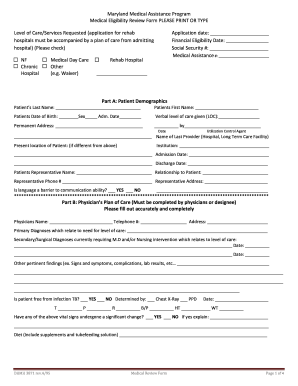
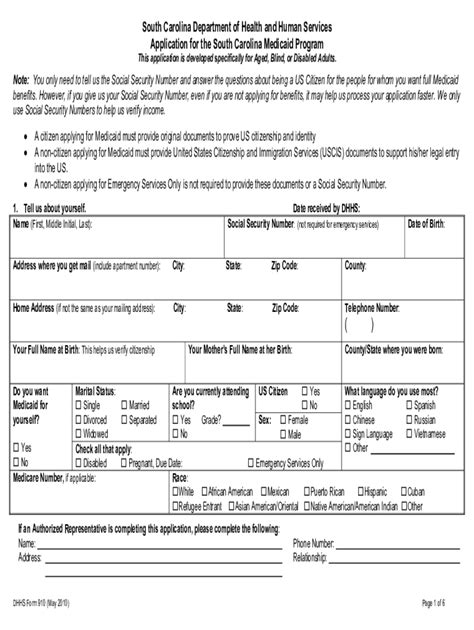
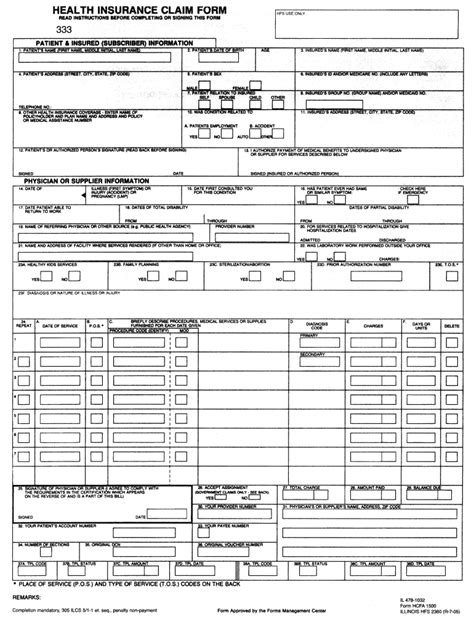
1. Medicaid Application Form (CMS-2556)
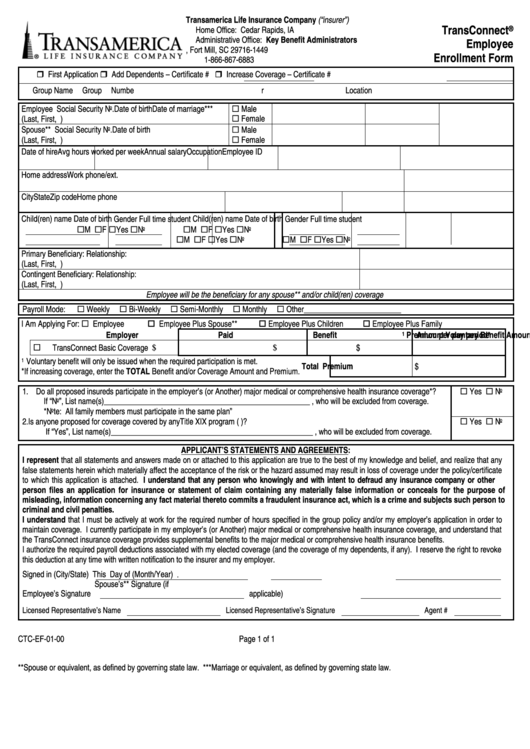
The Medicaid Application Form, also known as the CMS-2556, is the primary form used to apply for Medicaid benefits. This form requires applicants to provide personal and financial information, including income, assets, and family size. The information provided on this form helps determine an individual’s eligibility for Medicaid and the level of benefits they may receive. It’s essential to fill out this form accurately and completely to avoid delays or denial of benefits.
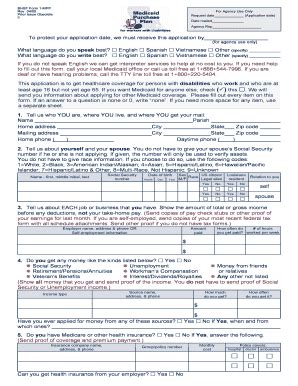
2. Medicaid Renewal Form
The Medicaid Renewal Form is used to renew Medicaid coverage for individuals who are already enrolled in the program. This form is typically sent to beneficiaries on a yearly basis and requires them to update their personal and financial information. The renewal form helps ensure that individuals continue to meet the eligibility requirements for Medicaid and receive the correct level of benefits. Failure to complete and return the renewal form may result in termination of Medicaid coverage.
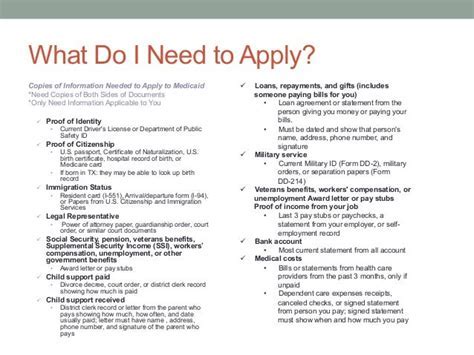
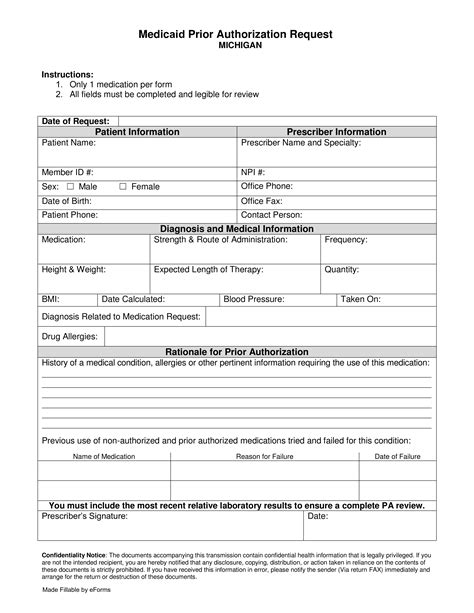
3. Medicaid Eligibility Verification Form
The Medicaid Eligibility Verification Form is used to verify an individual’s eligibility for Medicaid benefits. This form requires applicants to provide documentation, such as proof of income, citizenship, and identity, to support their application. The eligibility verification form helps ensure that only eligible individuals receive Medicaid benefits and prevents fraud and abuse.
4. Medicaid Appeal Form
The Medicaid Appeal Form is used to appeal a decision made by the Medicaid agency regarding an individual’s eligibility or benefits. This form allows individuals to dispute a decision they believe is incorrect or unfair and provides an opportunity for a fair hearing. The appeal form must be completed and submitted within a specified timeframe, typically 30 days, to ensure that the appeal is processed in a timely manner.
5. Medicaid Reporting Changes Form
The Medicaid Reporting Changes Form is used to report changes in an individual’s circumstances that may affect their Medicaid eligibility or benefits. This form requires beneficiaries to report changes, such as a new job, marriage, or divorce, within a specified timeframe, typically 10 days. Failing to report changes may result in termination of Medicaid coverage or incorrect benefits.
📝 Note: It's essential to review and understand the specific Medicaid forms required by your state, as they may vary. Additionally, individuals should seek assistance from a qualified healthcare professional or Medicaid representative if they need help completing the forms or have questions about the application and enrollment process.
In summary, understanding and completing the correct Medicaid forms is crucial for individuals seeking to apply for, renew, or appeal Medicaid benefits. By providing accurate and complete information on these forms, individuals can ensure they receive the correct level of benefits and avoid delays or termination of coverage.
What is the purpose of the Medicaid Application Form?
+
The Medicaid Application Form is used to apply for Medicaid benefits and determine an individual’s eligibility based on their income, assets, and family size.
How often do I need to renew my Medicaid coverage?
+
Medicaid coverage typically needs to be renewed on a yearly basis, and beneficiaries will receive a renewal form to update their personal and financial information.
What happens if I don’t report changes to my Medicaid eligibility?
+
Failing to report changes may result in termination of Medicaid coverage or incorrect benefits, so it’s essential to report changes promptly using the Medicaid Reporting Changes Form.