No Cobra Paperwork Received

Understanding COBRA and Its Importance
When an individual loses their job or experiences a reduction in work hours, they may be eligible for Consolidated Omnibus Budget Reconciliation Act (COBRA) benefits. COBRA is a federal law that allows certain employees and their families to continue their health insurance coverage temporarily. The law applies to employers with 20 or more employees, and it requires these employers to offer COBRA benefits to eligible employees and their dependents. If you have not received your COBRA paperwork, it is essential to understand the steps you can take to obtain the necessary documents and ensure you do not miss the opportunity to elect COBRA coverage.
Why Is COBRA Paperwork Important?
COBRA paperwork is crucial because it provides eligible individuals with the information they need to make informed decisions about their health insurance coverage. The paperwork typically includes details such as:
- The cost of COBRA coverage
- The duration of COBRA coverage
- The deadline for electing COBRA coverage
- Instructions for enrolling in COBRA
What to Do If You Haven’t Received COBRA Paperwork
If you are eligible for COBRA benefits and have not received the necessary paperwork, you should take the following steps:
- Contact your former employer’s HR department to inquire about the status of your COBRA paperwork
- Reach out to the plan administrator responsible for handling COBRA benefits for your former employer
- File a complaint with the U.S. Department of Labor if you believe your former employer has failed to provide you with the required COBRA paperwork
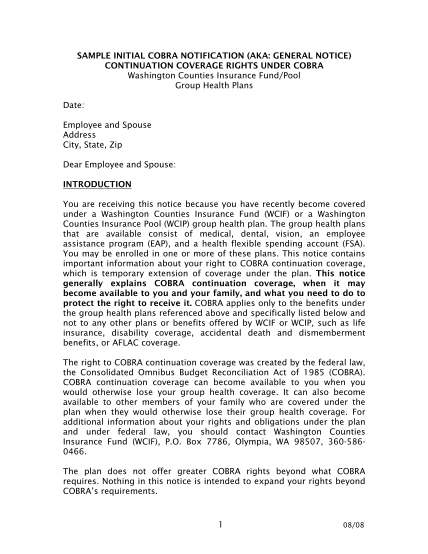
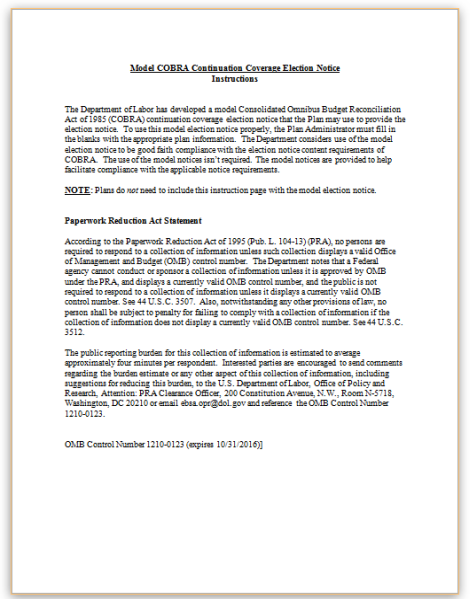
Understanding COBRA Election Notice
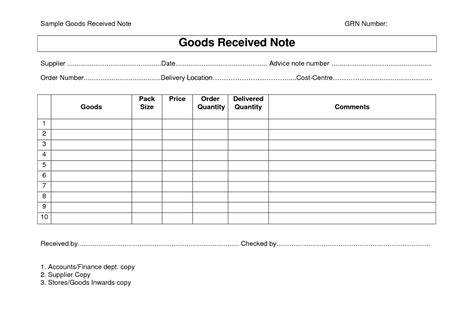
The COBRA election notice is a critical document that provides eligible individuals with the information they need to make informed decisions about their health insurance coverage. The notice should include the following details:
| Information | Description |
|---|---|
| Qualifying event | The reason for the loss of health insurance coverage (e.g., job loss, reduction in work hours) |
| COBRA coverage details | Information about the type of coverage available, including medical, dental, and vision |
| Cost of coverage | The premium amount and any other costs associated with COBRA coverage |
| Election deadline | The date by which you must elect COBRA coverage to avoid a gap in health insurance coverage |
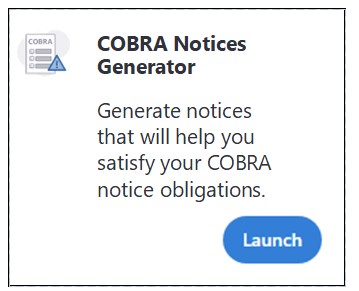
If you have not received a COBRA election notice, you should contact your former employer’s HR department or the plan administrator to request the necessary paperwork.
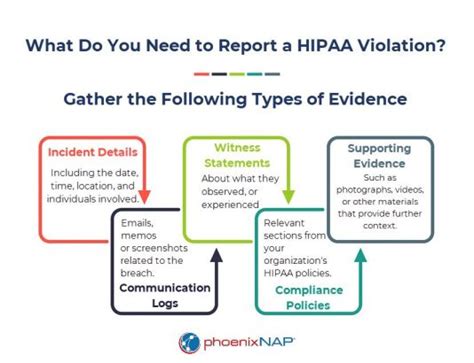
📝 Note: It is crucial to keep a record of all correspondence related to your COBRA benefits, including dates, times, and details of conversations with your former employer's HR department or the plan administrator.
COBRA Benefits and Eligibility
To be eligible for COBRA benefits, you must meet specific criteria, including:
- Qualifying event: You must have experienced a qualifying event, such as job loss, reduction in work hours, divorce, or death of the covered employee
- Employer size: Your former employer must have had 20 or more employees on at least 50% of its typical business days in the previous calendar year
- Coverage requirements: You must have been covered under your former employer’s health insurance plan on the day before the qualifying event
In summary, receiving COBRA paperwork is essential for eligible individuals to make informed decisions about their health insurance coverage. If you have not received your COBRA paperwork, you should contact your former employer’s HR department or the plan administrator to request the necessary documents. It is crucial to act promptly to avoid missing the deadline for electing COBRA coverage and to ensure you do not experience a gap in health insurance coverage.
What is COBRA, and how does it work?
+
COBRA is a federal law that allows certain employees and their families to continue their health insurance coverage temporarily after a qualifying event, such as job loss or reduction in work hours. COBRA requires employers with 20 or more employees to offer COBRA benefits to eligible employees and their dependents.
How long do I have to elect COBRA coverage?

+
You typically have 60 days from the date you receive the COBRA election notice to elect COBRA coverage. It is essential to act promptly to avoid missing the deadline and experiencing a gap in health insurance coverage.
What should I do if I haven’t received my COBRA paperwork?
+
If you haven’t received your COBRA paperwork, you should contact your former employer’s HR department or the plan administrator to request the necessary documents. You can also file a complaint with the U.S. Department of Labor if you believe your former employer has failed to provide you with the required COBRA paperwork.