Cobra Paperwork Arrival Timeline

Introduction to Cobra Paperwork Arrival Timeline

The Cobra paperwork arrival timeline is a crucial aspect of the Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985, which provides continuation of health coverage to employees and their families when they experience a qualifying event that would normally result in the loss of group health plan coverage. Understanding the timeline for the arrival of Cobra paperwork is essential for both employers and employees to ensure compliance with the law and to make informed decisions about health coverage.
Qualifying Events and Notification
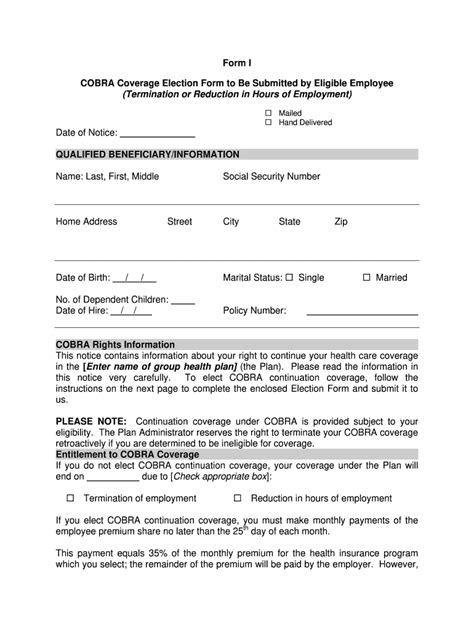
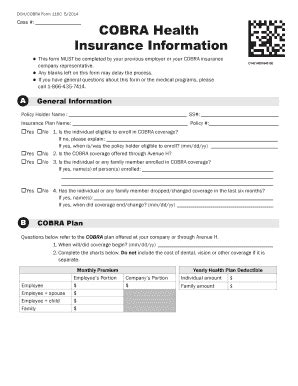
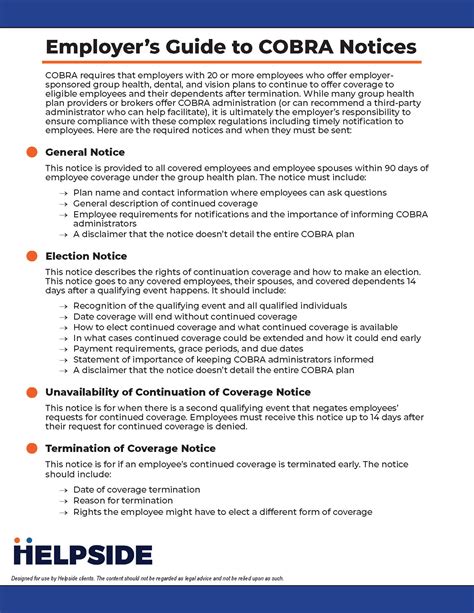
To initiate the Cobra paperwork process, a qualifying event must occur. Qualifying events include the death of the covered employee, termination or reduction in hours of the covered employee’s employment, divorce or legal separation from the covered employee, or a dependent child losing dependent status under the plan. When a qualifying event occurs, the employer or plan administrator must notify the affected individuals of their right to continue coverage under Cobra. This notification is typically made through a Cobra election notice, which outlines the terms and conditions of continued coverage, including the cost and duration of coverage.
Timeline for Cobra Paperwork Arrival
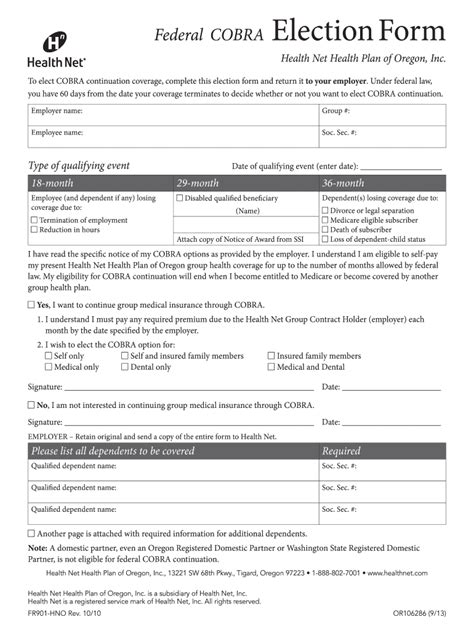
The timeline for the arrival of Cobra paperwork is as follows: - Qualifying Event Occurs: The process begins when a qualifying event occurs, triggering the need for Cobra coverage. - Notification Period: The employer or plan administrator has 30 days from the date of the qualifying event to notify the plan administrator of the event, if the event is the employee’s termination or reduction in hours. - Cobra Election Notice: The plan administrator then has 14 days from the date they receive the notification of the qualifying event to send the Cobra election notice to the qualified beneficiaries. - Election Period: Once the qualified beneficiaries receive the Cobra election notice, they have 60 days to decide whether to elect Cobra coverage. This 60-day election period begins on the date the notice is sent, not from the date the qualifying event occurred. - Premium Payment: After electing Cobra coverage, the first premium payment is due 45 days after the election. Subsequent payments are due on the first day of each month.
Key Considerations
It is crucial for both employers and qualified beneficiaries to understand and adhere to the Cobra paperwork arrival timeline. For employers, timely notification of qualifying events and the issuance of Cobra election notices are critical to avoid penalties and ensure compliance with Cobra regulations. For qualified beneficiaries, understanding the timeline is essential to make informed decisions about their health coverage options within the allowed timeframe.
Table of Cobra Timeline
| Event | Timeline | Description |
|---|---|---|
| Qualifying Event | Day 0 | Event that triggers Cobra, such as job termination. |
| Notification to Plan Administrator | Within 30 days | Employer notifies the plan administrator of the qualifying event. |
| Cobra Election Notice Sent | Within 14 days after notification | Plan administrator sends the Cobra election notice to qualified beneficiaries. |
| Cobra Election Period | 60 days from the notice date | Qualified beneficiaries decide whether to elect Cobra coverage. |
| First Premium Payment Due | 45 days after election | First premium payment for Cobra coverage is due. |
💡 Note: Understanding the Cobra timeline is crucial for compliance and making informed decisions about health coverage.
In summary, the Cobra paperwork arrival timeline is a structured process designed to ensure that qualified beneficiaries are informed and have the opportunity to continue their health coverage after a qualifying event. By understanding this timeline, individuals can navigate the process effectively, and employers can fulfill their obligations under the law.
What triggers the Cobra paperwork process?

+
A qualifying event, such as the death of the covered employee, termination or reduction in hours of the covered employee’s employment, divorce or legal separation from the covered employee, or a dependent child losing dependent status under the plan, triggers the Cobra paperwork process.
How long does the employer have to notify the plan administrator of a qualifying event?
+
The employer has 30 days from the date of the qualifying event to notify the plan administrator, if the event is the employee’s termination or reduction in hours.
What is the timeframe for qualified beneficiaries to decide whether to elect Cobra coverage?
+
Qualified beneficiaries have 60 days from the date the Cobra election notice is sent to decide whether to elect Cobra coverage.