COBRA Paperwork Deadline

Understanding COBRA Paperwork Deadline: A Comprehensive Guide
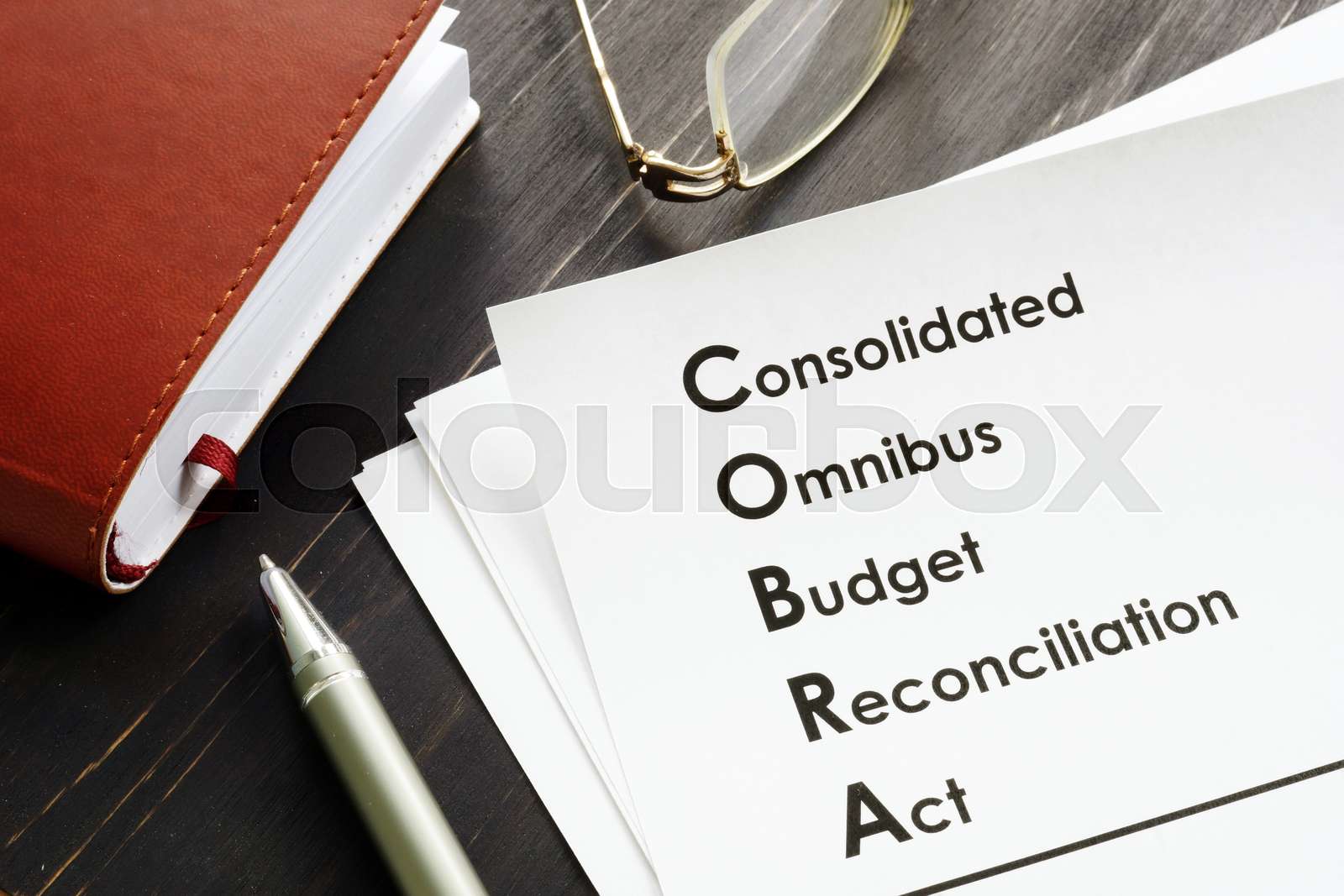
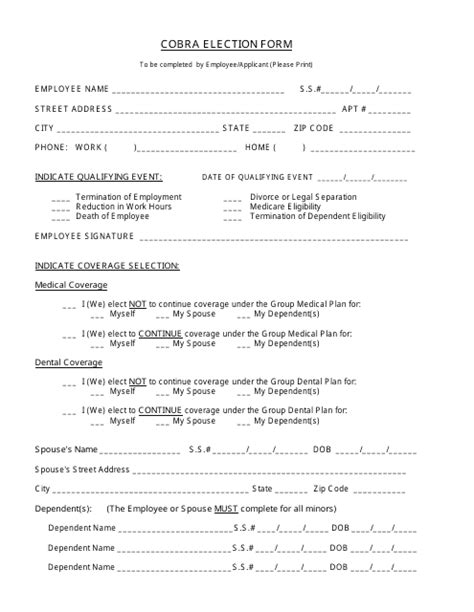
When an individual loses their job or experiences a reduction in work hours, they may be eligible for the Consolidated Omnibus Budget Reconciliation Act (COBRA) benefits. COBRA allows them to continue their group health coverage for a certain period. However, to qualify for these benefits, it’s essential to meet the COBRA paperwork deadline. In this article, we’ll delve into the world of COBRA, exploring the key aspects of the paperwork deadline and providing a step-by-step guide on how to navigate the process.
What is COBRA?

COBRA is a federal law that requires employers with 20 or more employees to offer continuing health coverage to employees and their families when they experience a qualifying event, such as job loss, reduction in work hours, divorce, or death of the covered employee. The law aims to provide temporary health coverage to individuals who would otherwise lose their group health benefits due to a qualifying event.
COBRA Paperwork Deadline: What You Need to Know
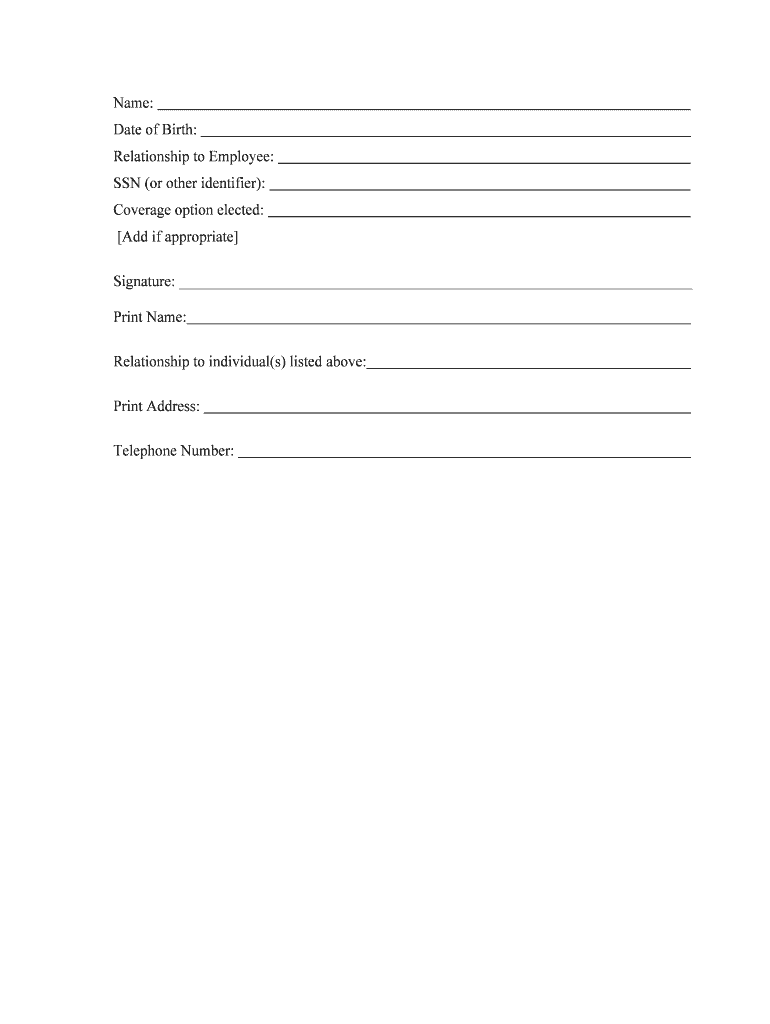
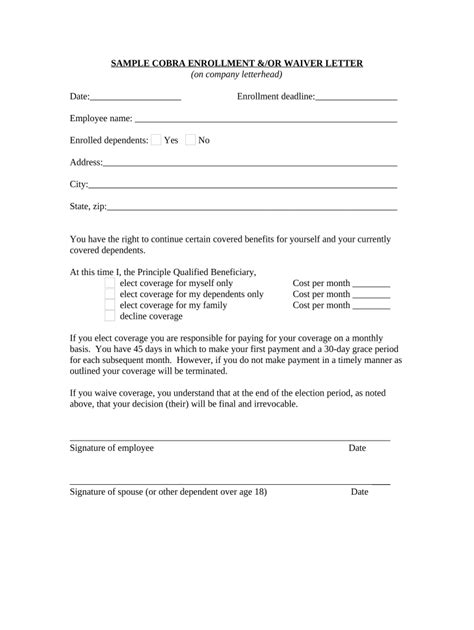
The COBRA paperwork deadline is a critical aspect of the COBRA benefits process. Generally, the employer must notify the plan administrator within 30 days of a qualifying event. The plan administrator then has 14 days to provide the qualified beneficiary with a COBRA election notice, which outlines their rights and obligations under COBRA. The qualified beneficiary has 60 days from the date of the election notice to elect COBRA coverage.
📝 Note: It's essential to review the COBRA election notice carefully, as it contains critical information about the COBRA benefits, including the premium amount, coverage period, and any applicable deadlines.
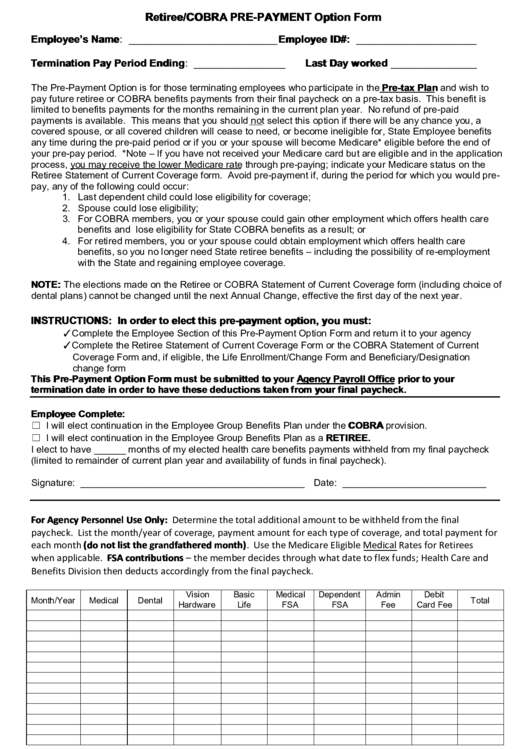
Step-by-Step Guide to Meeting the COBRA Paperwork Deadline
To ensure a smooth COBRA benefits process, follow these steps: * Step 1: Qualifying Event Notification: The employer must notify the plan administrator within 30 days of a qualifying event. * Step 2: COBRA Election Notice: The plan administrator has 14 days to provide the qualified beneficiary with a COBRA election notice. * Step 3: COBRA Election: The qualified beneficiary has 60 days from the date of the election notice to elect COBRA coverage. * Step 4: Premium Payment: The qualified beneficiary must pay the first premium within 45 days of electing COBRA coverage.
Key Considerations and Potential Pitfalls
When navigating the COBRA paperwork deadline, it’s crucial to be aware of the following: * Timing is Everything: Missing the COBRA paperwork deadline can result in the loss of COBRA benefits. * Communication is Key: Ensure that all parties involved, including the employer, plan administrator, and qualified beneficiary, are aware of their responsibilities and deadlines. * Premium Payments: The qualified beneficiary must make timely premium payments to maintain COBRA coverage.
Table: COBRA Paperwork Deadline Timeline
| Event | Deadline |
|---|---|
| Qualifying Event Notification | 30 days |
| COBRA Election Notice | 14 days |
| COBRA Election | 60 days |
| Premium Payment | 45 days |

In summary, meeting the COBRA paperwork deadline is critical to ensuring a smooth transition to COBRA benefits. By understanding the key aspects of the COBRA paperwork deadline and following the step-by-step guide, individuals can navigate the process with confidence. Remember to stay vigilant and communicate effectively with all parties involved to avoid potential pitfalls.
As we reflect on the importance of meeting the COBRA paperwork deadline, it’s clear that this process requires attention to detail and a thorough understanding of the COBRA benefits process. By being proactive and informed, individuals can ensure that they receive the continued health coverage they need during a time of transition.
What is the COBRA paperwork deadline for electing coverage?
+
The qualified beneficiary has 60 days from the date of the election notice to elect COBRA coverage.
What happens if I miss the COBRA paperwork deadline?
+
Missing the COBRA paperwork deadline can result in the loss of COBRA benefits. It’s essential to meet the deadline to ensure continued health coverage.
How do I make premium payments for COBRA coverage?
+
The qualified beneficiary must make timely premium payments to maintain COBRA coverage. The first premium payment is due within 45 days of electing COBRA coverage.