Meicaid Provider Paperwork Filing Help
Introduction to Medicaid Provider Paperwork Filing
Medicaid is a state and federally funded program that provides health coverage to eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. As a Medicaid provider, navigating the complex process of filing paperwork can be overwhelming. From enrollment to reimbursement, the administrative tasks involved in Medicaid provider paperwork can be time-consuming and require a significant amount of resources. In this blog post, we will explore the world of Medicaid provider paperwork filing, providing guidance and support to help providers manage their administrative tasks more efficiently.
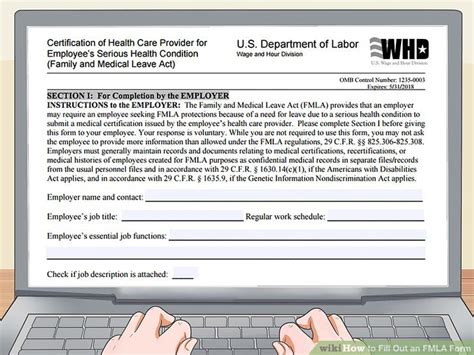
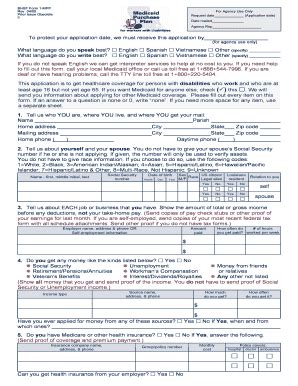
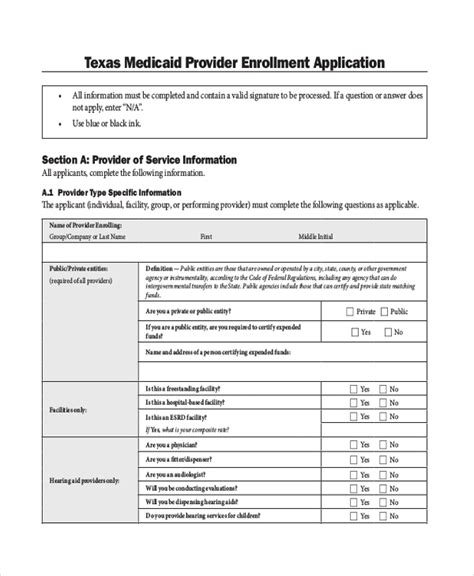
Understanding Medicaid Provider Enrollment
The first step in becoming a Medicaid provider is to enroll in the program. This involves submitting an application, which includes providing detailed information about the practice, such as business name, address, and tax identification number. It is essential to ensure that all information is accurate and up-to-date to avoid delays in the enrollment process. Additionally, providers must meet specific requirements, such as having a valid medical license and malpractice insurance. The enrollment process can be complex, and it is crucial to understand the requirements and regulations governing Medicaid provider enrollment.
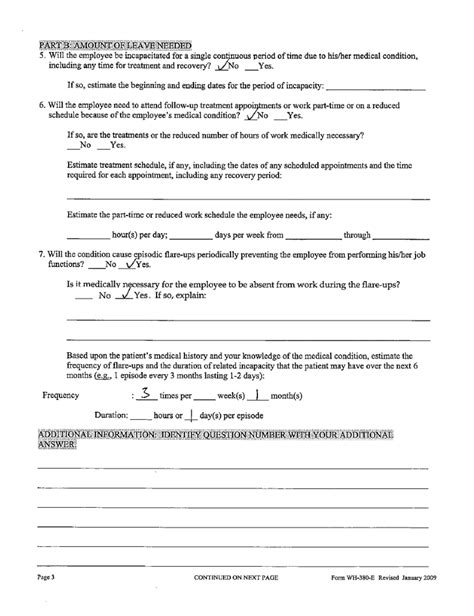
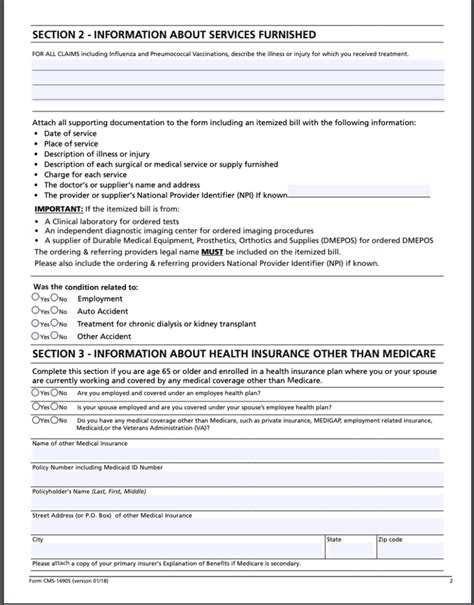
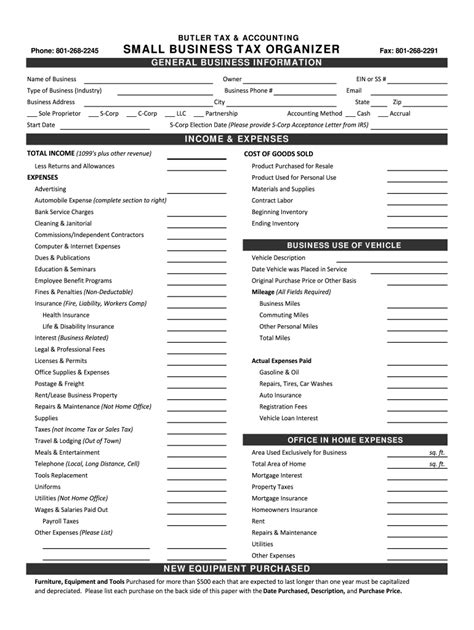
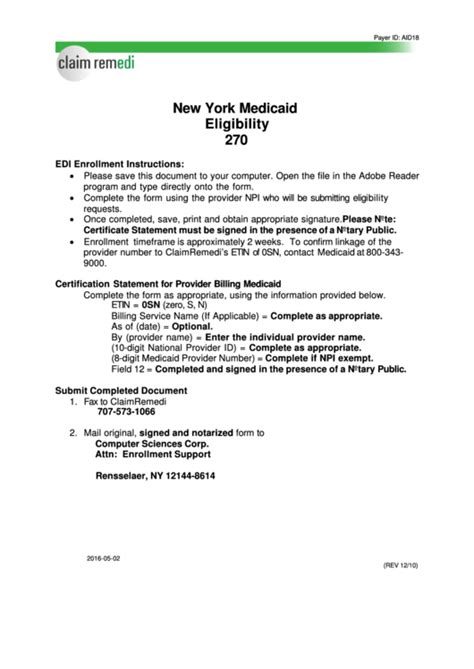
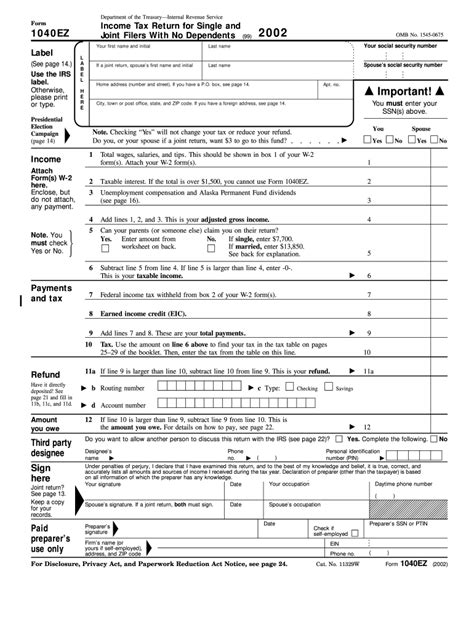
Medicaid Claim Submission Process
Once enrolled, providers must submit claims for services rendered to Medicaid beneficiaries. The claim submission process involves completing a claim form, which includes providing detailed information about the service, such as diagnosis codes, procedure codes, and charges. Accurate and timely submission of claims is critical to ensuring reimbursement. Providers can submit claims electronically or by mail, and it is essential to follow the guidelines and regulations set by the state Medicaid agency.
Types of Medicaid Claims

There are several types of Medicaid claims, including: * Inpatient claims: Claims for services provided to patients who are hospitalized. * Outpatient claims: Claims for services provided to patients who are not hospitalized. * Professional claims: Claims for services provided by healthcare professionals, such as physicians and nurse practitioners. * Institutional claims: Claims for services provided by institutions, such as hospitals and nursing homes.
Medicaid Reimbursement Process

The reimbursement process involves reviewing and processing claims submitted by providers. The state Medicaid agency reviews claims to ensure that they meet the requirements and regulations governing Medicaid reimbursement. Providers can expect to receive reimbursement for approved claims, which can be electronically deposited into their bank accounts or sent by mail.
Common Challenges in Medicaid Provider Paperwork Filing

Despite the importance of Medicaid provider paperwork filing, many providers face challenges in managing their administrative tasks. Some common challenges include: * Delays in claim processing: Delays in claim processing can result in delayed reimbursement, which can impact a provider’s cash flow. * Denied claims: Denied claims can result in lost revenue and require providers to resubmit claims, which can be time-consuming. * Lack of transparency: Lack of transparency in the claim submission and reimbursement process can make it difficult for providers to track the status of their claims.
📝 Note: Providers can avoid common challenges by ensuring that they have a thorough understanding of the Medicaid provider paperwork filing process and by staying up-to-date with the latest regulations and guidelines.
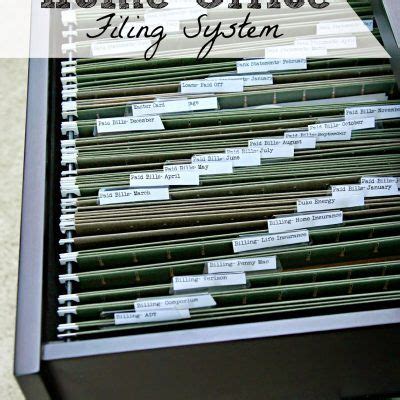
Best Practices for Medicaid Provider Paperwork Filing
To manage Medicaid provider paperwork filing more efficiently, providers can follow best practices, such as: * Staying organized: Keeping track of claims and reimbursement can help providers identify issues and resolve them quickly. * Using electronic claim submission: Electronic claim submission can reduce errors and improve the efficiency of the claim submission process. * Verifying beneficiary eligibility: Verifying beneficiary eligibility can help providers avoid denied claims and ensure that they receive reimbursement for services rendered.
Conclusion

In conclusion, Medicaid provider paperwork filing is a complex process that requires a significant amount of resources and attention to detail. By understanding the requirements and regulations governing Medicaid provider enrollment, claim submission, and reimbursement, providers can manage their administrative tasks more efficiently. Additionally, following best practices, such as staying organized and using electronic claim submission, can help providers avoid common challenges and ensure that they receive reimbursement for services rendered.
What is the Medicaid provider enrollment process?
+
The Medicaid provider enrollment process involves submitting an application, which includes providing detailed information about the practice, such as business name, address, and tax identification number.
How do I submit a Medicaid claim?
+
Medicaid claims can be submitted electronically or by mail. Providers must complete a claim form, which includes providing detailed information about the service, such as diagnosis codes, procedure codes, and charges.
What are the common challenges in Medicaid provider paperwork filing?

+
Common challenges in Medicaid provider paperwork filing include delays in claim processing, denied claims, and lack of transparency in the claim submission and reimbursement process.