COBRA Paperwork Deadline
Understanding COBRA Paperwork Deadline
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that allows certain employees and their families to temporarily continue their health coverage after a qualifying event, such as job loss or reduction in working hours. One of the critical aspects of COBRA is meeting the paperwork deadline to ensure continuity of health insurance coverage. In this article, we will delve into the details of COBRA paperwork deadlines, the process of applying, and the importance of adhering to these timelines.
Qualifying Events and Eligibility
To be eligible for COBRA, an individual must experience a qualifying event, which includes: - Voluntary or involuntary termination of employment for reasons other than gross misconduct - Reduction in hours of work - Divorce or legal separation from the covered employee - Death of the covered employee - Dependent child ceasing to be a dependent under the plan These events trigger the opportunity for the affected individuals to continue their health coverage under COBRA.
COBRA Paperwork Deadline
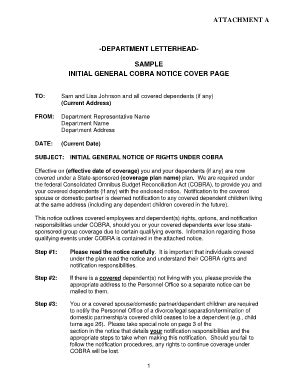
Upon experiencing a qualifying event, the employer or plan administrator must provide the affected individual with a COBRA election notice within 60 days after the qualifying event or the date coverage would otherwise end, whichever is later. This notice includes crucial information about the individual’s rights under COBRA, the cost of coverage, and the deadline by which they must respond to the notice.
The individual then has 60 days from the date the notice is provided (or the date coverage would otherwise end) to decide whether to elect COBRA coverage. It is essential to carefully review the notice and understand the implications of electing or declining COBRA coverage. If the individual decides to elect COBRA, they must complete and return the election form by the specified deadline.
Process of Applying for COBRA
The process of applying for COBRA involves the following steps: - Receiving the COBRA Election Notice: The employer or plan administrator sends the notice to the eligible individual. - Reviewing the Notice: The individual reviews the notice to understand their rights, the cost of coverage, and the deadline for responding. - Deciding on Coverage: The individual decides whether to elect COBRA coverage within the 60-day timeframe. - Completing the Election Form: If electing coverage, the individual completes and returns the election form by the deadline. - Payment of Premiums: The individual begins paying the required premiums to maintain COBRA coverage.
Importance of Meeting the Deadline

Meeting the COBRA paperwork deadline is crucial to avoid a gap in health insurance coverage. Failure to respond to the election notice within the specified timeframe may result in the loss of COBRA eligibility. Given the potential consequences of missing this deadline, including loss of health coverage and the possibility of being uninsured, it is vital for individuals to act promptly upon receiving the COBRA election notice.
📝 Note: Individuals should carefully review their COBRA election notice and seek advice if they are unsure about any aspect of the process to ensure they make informed decisions about their health coverage.
Conclusion and Key Points

In summary, understanding and meeting the COBRA paperwork deadline is essential for individuals who experience a qualifying event and wish to continue their health insurance coverage. Key points to remember include the importance of responding to the COBRA election notice within the 60-day timeframe, carefully reviewing the notice to understand the implications of electing or declining coverage, and seeking advice if unsure about any aspect of the COBRA process. By being informed and proactive, individuals can navigate the COBRA process effectively and maintain their health coverage during a critical period.
What is the purpose of COBRA?
+
The purpose of COBRA is to allow certain employees and their families to temporarily continue their health coverage after a qualifying event, such as job loss or reduction in working hours.
How long do I have to elect COBRA coverage after receiving the election notice?

+
You have 60 days from the date the notice is provided (or the date coverage would otherwise end) to decide whether to elect COBRA coverage.
What happens if I miss the deadline to elect COBRA coverage?

+
If you miss the deadline to elect COBRA coverage, you may lose your eligibility for COBRA and face a gap in your health insurance coverage.