5 Endoscopy Consent Facts
Introduction to Endoscopy Consent
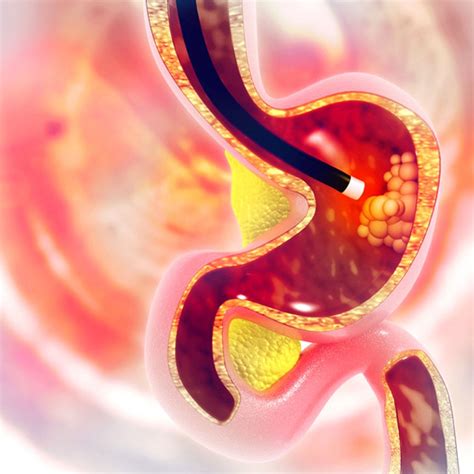
Endoscopy is a medical procedure that involves the use of a flexible tube with a camera and light on the end to visualize the inside of the body. It is used to diagnose and treat a variety of conditions, including gastrointestinal problems, respiratory issues, and joint pain. Before undergoing an endoscopy, patients are required to provide informed consent, which is a crucial aspect of the procedure. Informed consent ensures that patients are aware of the risks, benefits, and alternatives to the procedure, and that they make an informed decision about whether to proceed. In this article, we will discuss five important facts about endoscopy consent that patients should know.
Fact 1: Understanding the Risks and Benefits
Before providing consent, patients should have a clear understanding of the risks and benefits associated with the endoscopy procedure. The risks may include bleeding, infection, and perforation of the organ being examined. The benefits, on the other hand, may include accurate diagnosis, effective treatment, and improved symptoms. Patients should discuss these risks and benefits with their doctor to determine whether the procedure is right for them. It is essential to ask questions and express any concerns to ensure that patients are fully informed.
Fact 2: Alternatives to Endoscopy
Patients should be aware of the alternatives to endoscopy, which may include other diagnostic tests or procedures. For example, imaging tests such as X-rays, CT scans, or MRI scans may be used to diagnose certain conditions. In some cases, medication or other treatments may be used to manage symptoms instead of undergoing an endoscopy. Patients should discuss these alternatives with their doctor to determine the best course of treatment for their specific condition.
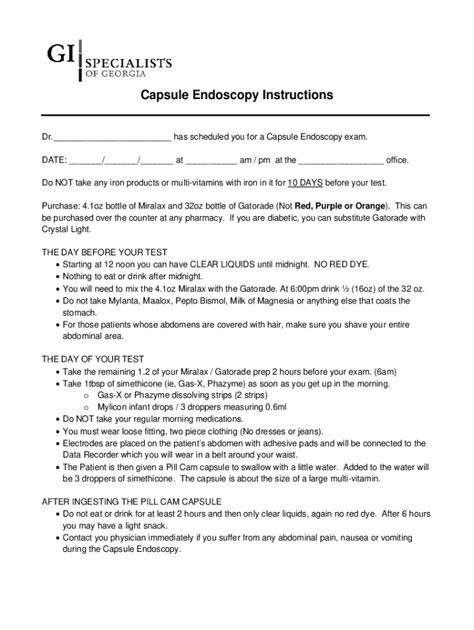
Fact 3: The Consent Process
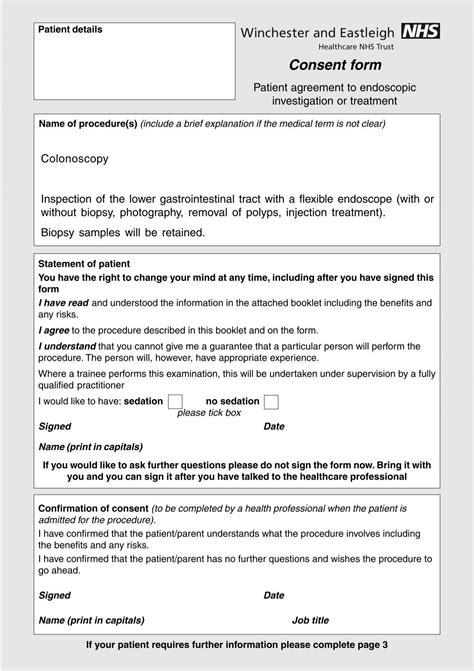
The consent process typically involves a discussion between the patient and their doctor, during which the doctor explains the procedure, the risks and benefits, and the alternatives. Patients should be given the opportunity to ask questions and express any concerns they may have. The doctor should also provide patients with written information about the procedure, which may include a consent form that outlines the details of the procedure and the risks and benefits. Patients should read this information carefully and ask questions if they do not understand anything.
Fact 4: Withdrawing Consent

Patients have the right to withdraw their consent at any time, even after the procedure has started. If a patient decides to withdraw their consent, the procedure will be stopped, and alternative treatments will be discussed. Patients should not feel pressured to proceed with the procedure if they are unsure or have changed their mind. It is essential to communicate openly and honestly with the doctor and medical team to ensure that patients receive the best possible care.
Fact 5: Special Considerations
There may be special considerations for certain patients, such as those with disabilities, language barriers, or cognitive impairments. In these cases, patients may require additional support or accommodations to ensure that they can provide informed consent. For example, interpretation services may be provided for patients who do not speak the same language as their doctor. Patients should inform their doctor of any special needs or requirements to ensure that they receive the necessary support.
📝 Note: Patients should keep a copy of their consent form and any other relevant documents for their records.
In summary, endoscopy consent is a critical aspect of the procedure, and patients should be fully informed about the risks, benefits, and alternatives. By understanding these five important facts, patients can make an informed decision about whether to undergo an endoscopy and ensure that they receive the best possible care. Patients should always prioritize their health and well-being by asking questions, expressing concerns, and seeking support when needed.
What is the purpose of informed consent in endoscopy?
+
The purpose of informed consent is to ensure that patients are aware of the risks, benefits, and alternatives to the procedure, and that they make an informed decision about whether to proceed.
Can patients withdraw their consent after the procedure has started?
+
Yes, patients have the right to withdraw their consent at any time, even after the procedure has started. If a patient decides to withdraw their consent, the procedure will be stopped, and alternative treatments will be discussed.
What should patients do if they have concerns or questions about the endoscopy procedure?
+
Patients should discuss their concerns or questions with their doctor or medical team. It is essential to communicate openly and honestly to ensure that patients receive the best possible care.