5 Diagnosis Forms
Introduction to Diagnosis Forms

Diagnosis forms are essential tools in the medical field, used by healthcare professionals to gather information about a patient’s condition, symptoms, and medical history. These forms help doctors and nurses to diagnose and treat patients effectively. In this article, we will explore five common diagnosis forms used in various medical settings.
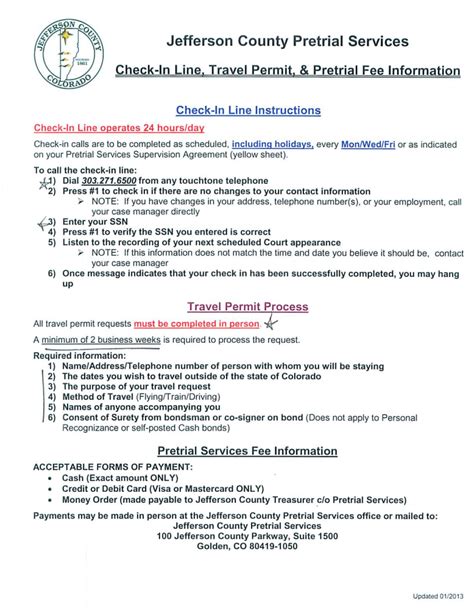
1. Patient Intake Form

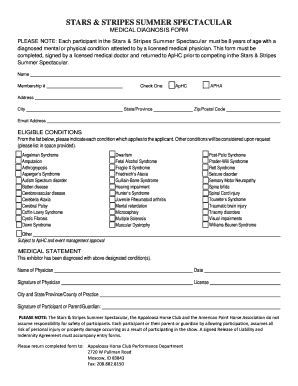
The patient intake form is the most basic diagnosis form, used to collect general information about a patient. This form typically includes:
- Personal details: name, age, address, and contact information
- Medical history: previous illnesses, allergies, and surgeries
- Current symptoms: description of the patient’s condition and symptoms
- Medications: list of current medications and dosages
2. Review of Systems (ROS) Form
The Review of Systems (ROS) form is a comprehensive diagnosis form used to evaluate a patient’s symptoms and medical history. This form is divided into sections, each focusing on a specific system of the body, such as:
- Cardiovascular system
- Respiratory system
- Gastrointestinal system
- Nervous system
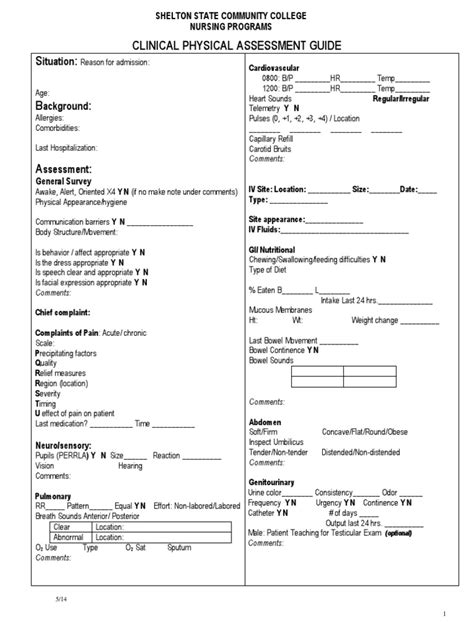
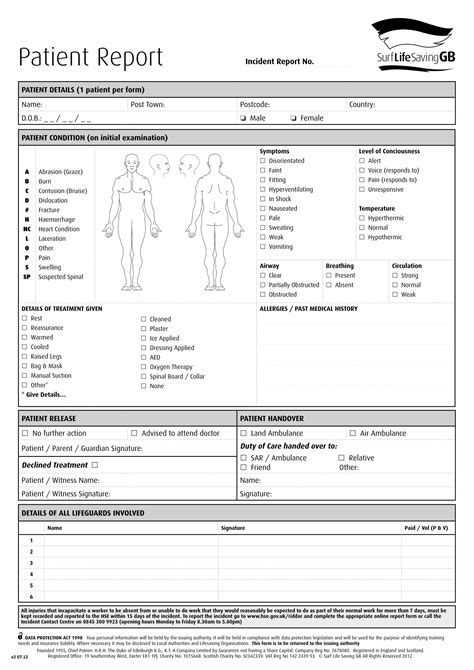
3. Physical Examination Form
The physical examination form is used to document the results of a physical examination. This form typically includes:
- Vital signs: temperature, blood pressure, pulse, and respiratory rate
- General appearance: observation of the patient’s overall condition
- Head and neck examination: evaluation of the eyes, ears, nose, and throat
- Body system examination: evaluation of the cardiovascular, respiratory, gastrointestinal, and nervous systems
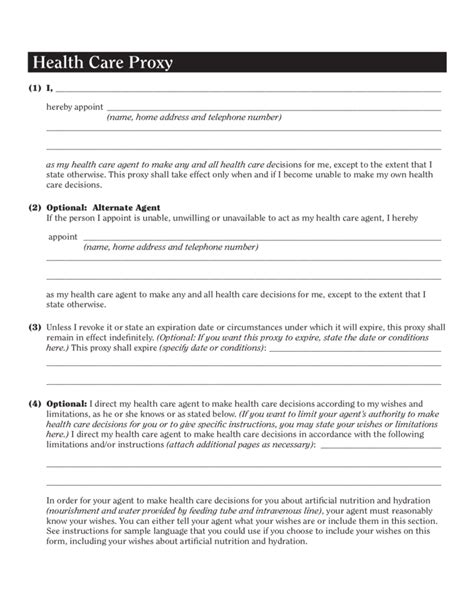
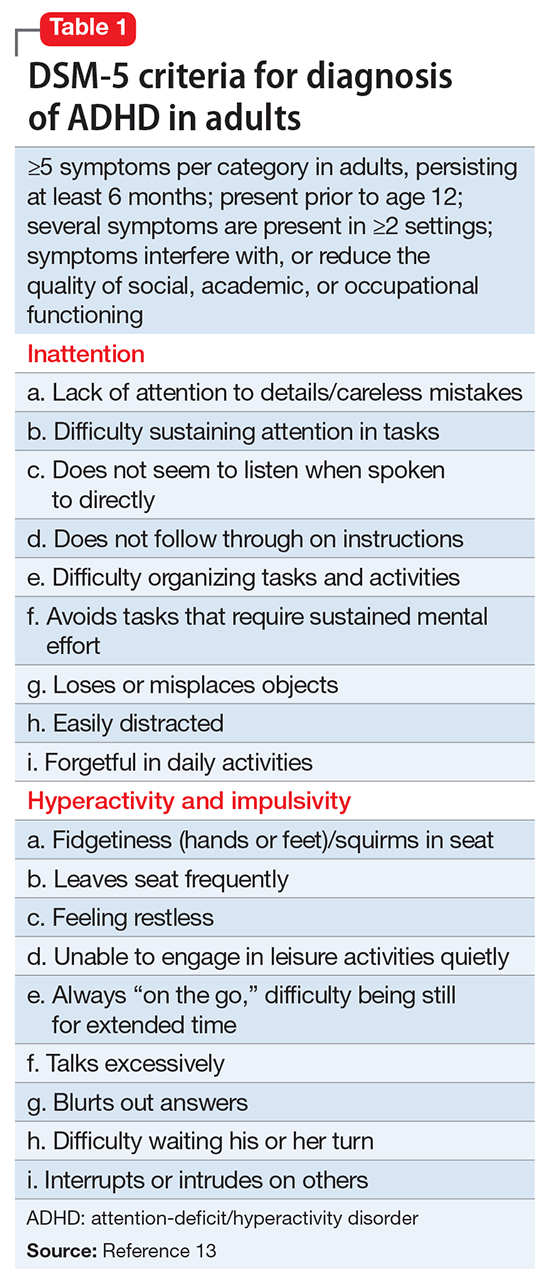
4. Mental Status Examination (MSE) Form
The Mental Status Examination (MSE) form is used to evaluate a patient’s cognitive and emotional function. This form typically includes:
- Level of consciousness: assessment of the patient’s alertness and awareness
- Orientation: evaluation of the patient’s ability to identify themselves, their location, and the current date and time
- Memory: assessment of the patient’s short-term and long-term memory
- Mood and affect: evaluation of the patient’s emotional state
5. Laboratory Results Form
The laboratory results form is used to document the results of laboratory tests, such as blood work and imaging studies. This form typically includes:
- Test results: documentation of the results of laboratory tests
- Normal ranges: comparison of the patient’s test results to normal ranges
- Abnormal results: identification of abnormal test results and potential causes
💡 Note: These forms are not exhaustive, and healthcare professionals may use additional forms and tools to diagnose and treat patients.
In summary, diagnosis forms are essential tools in the medical field, used to gather information about a patient’s condition, symptoms, and medical history. The five diagnosis forms discussed in this article - patient intake form, Review of Systems (ROS) form, physical examination form, Mental Status Examination (MSE) form, and laboratory results form - are commonly used in various medical settings to diagnose and treat patients effectively. By using these forms, healthcare professionals can develop a comprehensive understanding of a patient’s condition and provide high-quality care.
What is the purpose of a patient intake form?

+
The purpose of a patient intake form is to collect general information about a patient, including their personal details, medical history, and current symptoms.
What is the difference between a Review of Systems (ROS) form and a physical examination form?
+
A Review of Systems (ROS) form is used to evaluate a patient’s symptoms and medical history, while a physical examination form is used to document the results of a physical examination.
Why is it important to use diagnosis forms in medical settings?

+
Diagnosis forms are important because they help healthcare professionals to gather information about a patient’s condition, symptoms, and medical history, and to develop a diagnosis and treatment plan.