No Cobra Paperwork Received
Understanding COBRA and Its Importance
When an individual leaves a job, either voluntarily or involuntarily, one of the primary concerns is the potential loss of health insurance coverage. The Consolidated Omnibus Budget Reconciliation Act of 1985, commonly known as COBRA, is a federal law that allows certain former employees, retirees, spouses, former spouses, and dependent children to temporarily continue their health coverage at group rates. This coverage, however, is only available when the individual experiences a qualifying event, such as job loss, divorce, death of the covered employee, or a child losing dependent status.
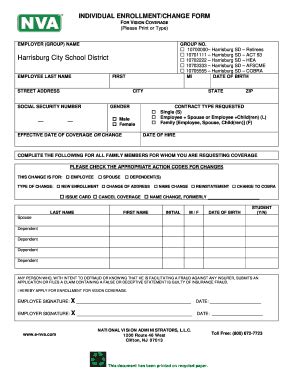
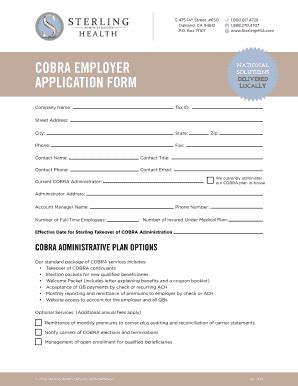
The COBRA Process
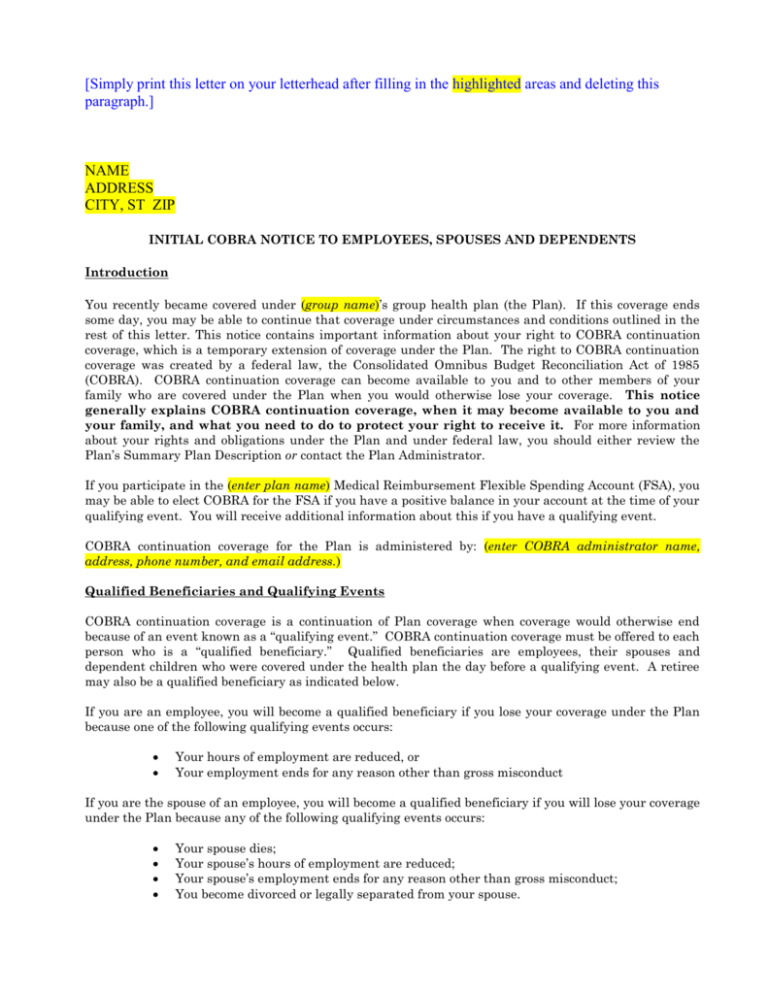
For those eligible, the process of enrolling in COBRA typically begins with the employer or the plan administrator notifying the qualified beneficiaries of their rights under COBRA. This notification is crucial as it informs the beneficiaries about their eligibility, the cost of the coverage, how to elect the coverage, and the time frame within which they must make this election. The notice must be provided in writing and is usually sent via mail. The employer or plan administrator has a specific time frame, usually 44 days from the qualifying event or the date the employer learns of the qualifying event, to send out this initial notice.
What to Do If You Haven’t Received COBRA Paperwork

If you believe you are eligible for COBRA coverage but haven’t received the necessary paperwork, there are several steps you can take: - Contact Your Former Employer or HR Department: Reach out to your former employer’s human resources department or the person responsible for benefits administration to inquire about the status of your COBRA notification. Be prepared to provide your name, the date you left the company, and a brief description of your situation. - Check with the Plan Administrator: If your former employer is unresponsive or unable to assist, you may need to contact the plan administrator directly. This information should be available through your former employer or on your health insurance card. - Review Your Records: Ensure that your former employer has your correct mailing address. Sometimes, notifications are sent but not received due to incorrect contact information. - Seek Professional Advice: If you continue to encounter difficulties, consulting with a benefits expert or an attorney specializing in employment law may provide additional guidance tailored to your situation.
Why COBRA Might Be Delayed
There are several reasons why you might not have received your COBRA paperwork: - Administrative Delays: The process of notifying beneficiaries can sometimes be slow due to the administrative burden on employers or plan administrators. - Change in Employment Status: If your employment status changed recently, it might take some time for the necessary paperwork to be processed. - Eligibility Issues: There could be questions regarding your eligibility for COBRA, which might delay the notification process.
Important Considerations

- Election Period: Once you receive the COBRA notice, you typically have 60 days to decide whether to elect COBRA coverage. This period begins on the later of the date of the COBRA notice or the date your health coverage would otherwise end due to the qualifying event. - Premium Payments: To maintain COBRA coverage, you must pay the premiums on time. The first premium payment is usually due 45 days after you elect COBRA coverage, and it may include the premium for the period of coverage from the date your previous coverage ended. - Alternative Coverage Options: While awaiting COBRA paperwork or considering the cost of COBRA premiums, it might be beneficial to explore other health insurance options, such as plans available through the Health Insurance Marketplace or a spouse’s plan, if available.
📝 Note: It's essential to keep detailed records of all communications regarding your COBRA eligibility and any issues that arise during the process.
In the event that you’re struggling to obtain your COBRA paperwork or have questions about the process, persistence and seeking the right guidance are key. The laws surrounding COBRA are in place to protect individuals during significant life changes, ensuring they have access to essential health coverage.
As we summarize the key aspects of dealing with unreceived COBRA paperwork, it’s clear that understanding your rights, being proactive in seeking information, and exploring all available health insurance options are crucial steps in navigating this often complex process. Whether you’re dealing with the immediate aftermath of a job change or planning for future scenarios, being informed about COBRA and its applications can provide significant peace of mind and financial protection.
What is the primary purpose of COBRA?
+
The primary purpose of COBRA is to allow certain former employees, retirees, spouses, former spouses, and dependent children to temporarily continue their health coverage at group rates after experiencing a qualifying event.
How long do I have to elect COBRA coverage after receiving the notice?
+
You typically have 60 days to decide whether to elect COBRA coverage after receiving the notice.
What should I do if I haven’t received my COBRA paperwork?
+
If you believe you are eligible for COBRA coverage but haven’t received the necessary paperwork, contact your former employer or the plan administrator to inquire about the status of your COBRA notification.