5 Therapy Forms
Introduction to Therapy Forms
Therapy forms are essential tools used by mental health professionals to assess, diagnose, and treat their clients. These forms help therapists to gather relevant information about their clients’ mental health, behaviors, and emotions, which is crucial in developing an effective treatment plan. In this article, we will discuss five common therapy forms used in the field of mental health.
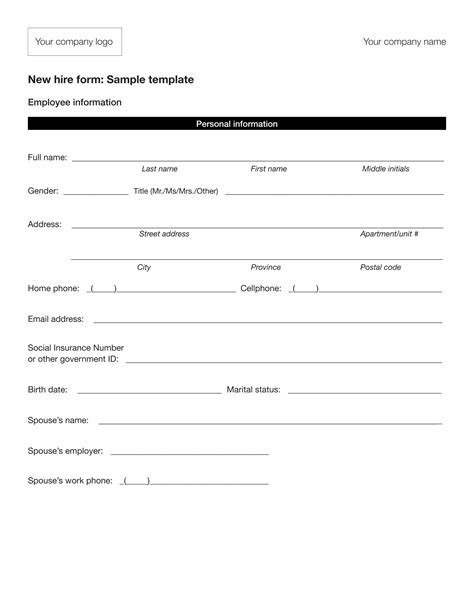
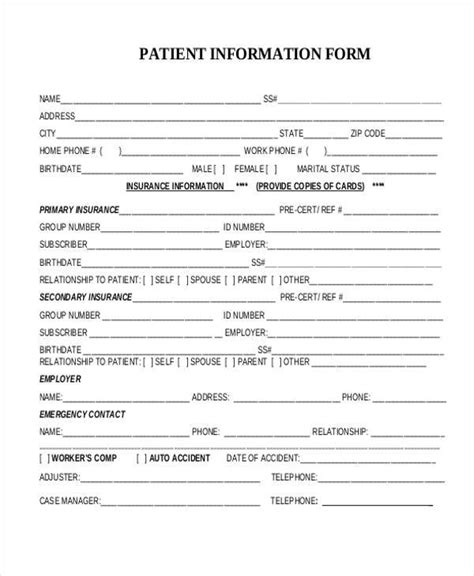
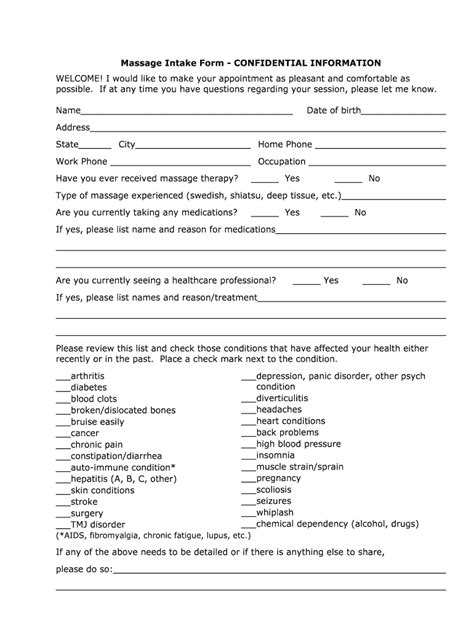
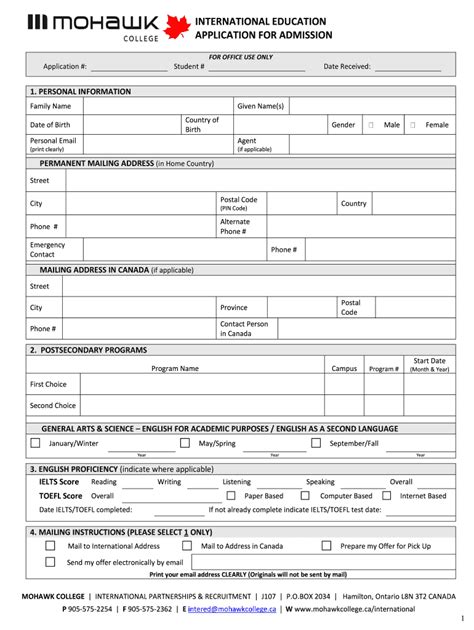
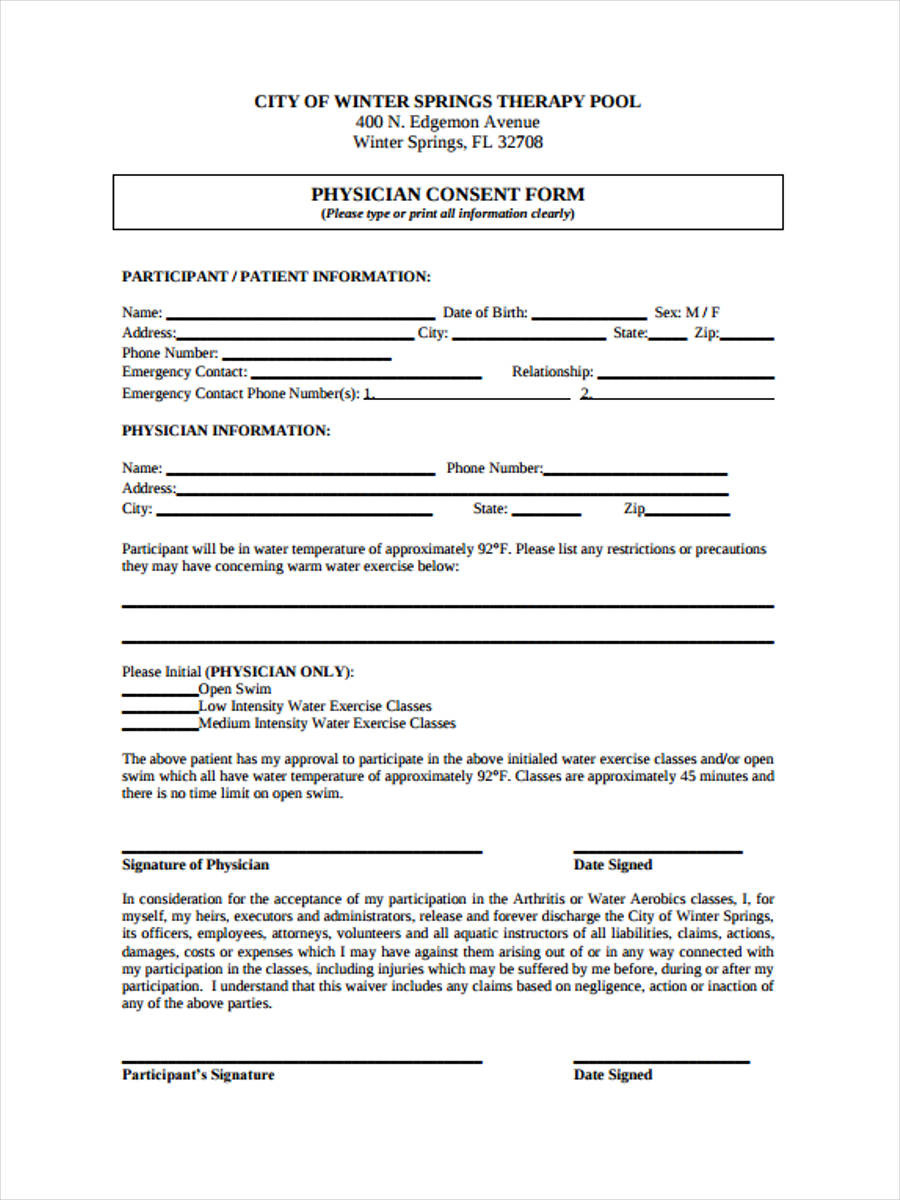
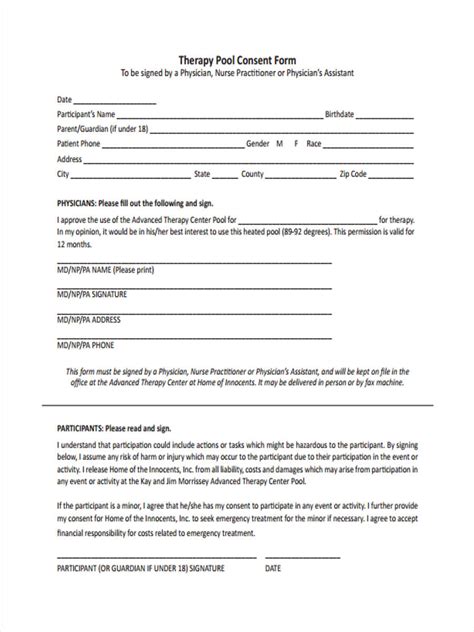
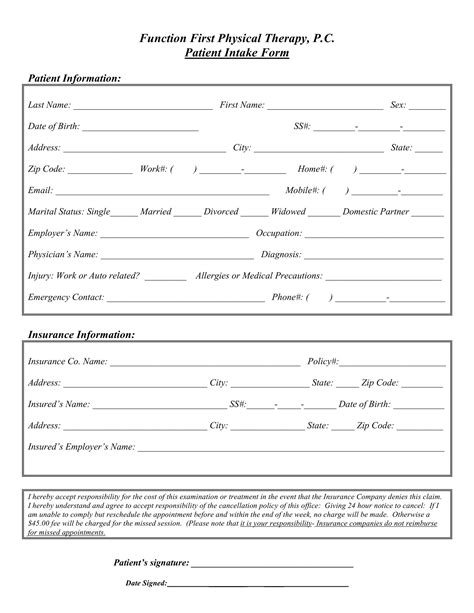
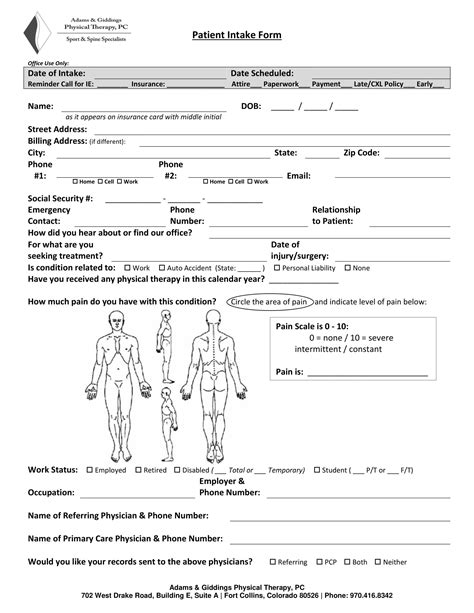
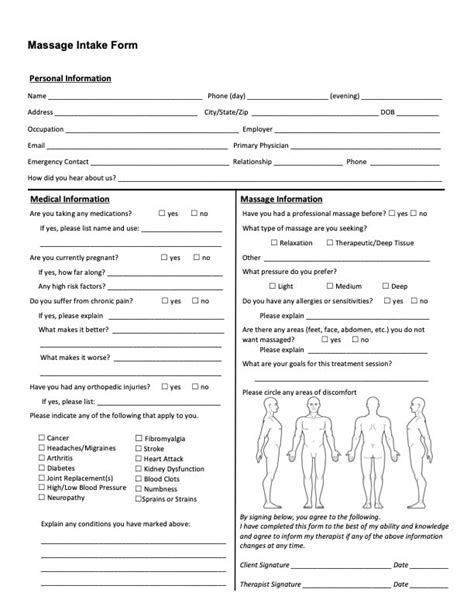
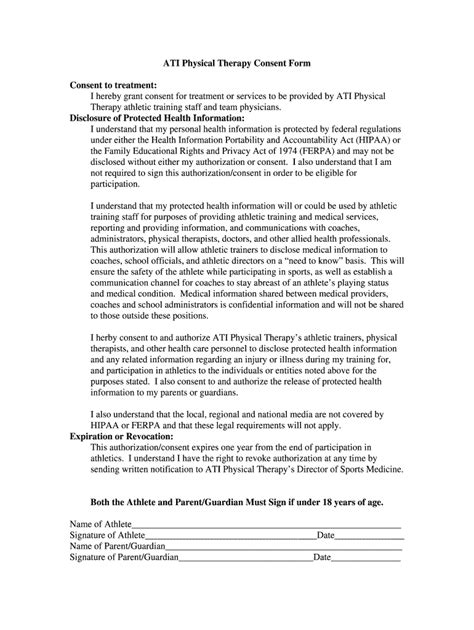
1. Client Intake Form
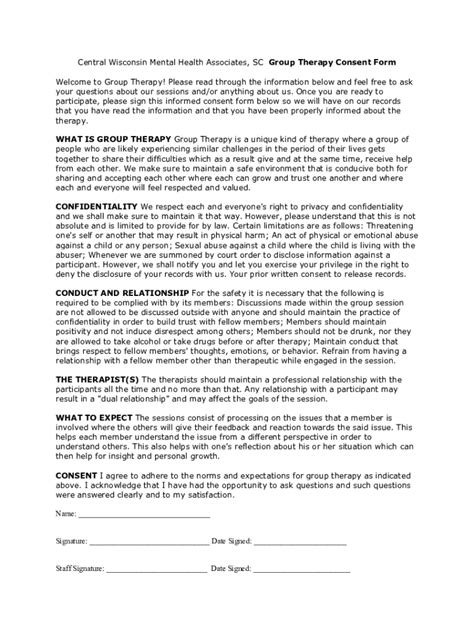
A client intake form is a document that clients fill out before their first therapy session. This form typically includes basic demographic information, such as name, age, and contact details, as well as questions about the client’s mental health history, including any previous therapy or counseling experiences. The form may also ask about the client’s reasons for seeking therapy, their goals for treatment, and any medications they are currently taking.
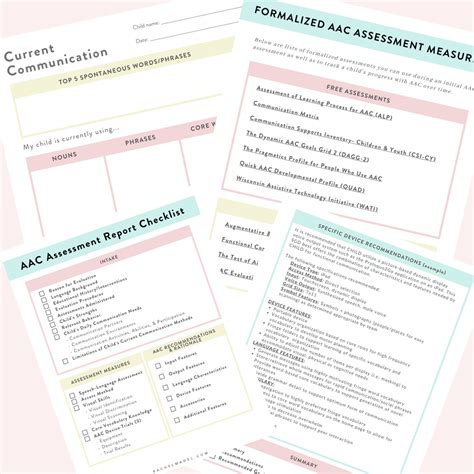
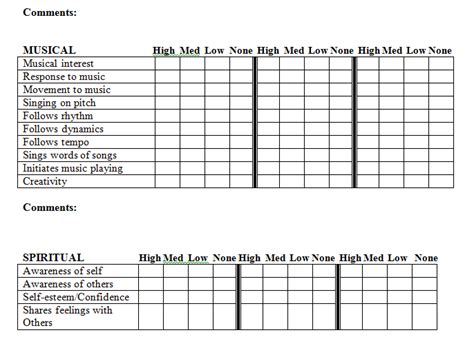
2. Behavioral Assessment Form
A behavioral assessment form is used to evaluate a client’s behaviors, thoughts, and feelings. This form may include questions about the client’s daily routines, social relationships, and coping mechanisms, as well as any symptoms of mental health conditions such as anxiety, depression, or trauma. The form may also include standardized assessment tools, such as the Beck Depression Inventory or the Hamilton Anxiety Rating Scale.
3. Treatment Plan Form
A treatment plan form is used to outline the client’s goals, objectives, and interventions for therapy. This form typically includes information about the client’s diagnosis, treatment modalities, and expected outcomes. The form may also include space for the therapist to note progress, setbacks, and any changes to the treatment plan.
4. Progress Notes Form
A progress notes form is used to document the client’s progress in therapy. This form typically includes space for the therapist to note the date, time, and duration of each session, as well as the client’s symptoms, behaviors, and emotions. The form may also include space for the therapist to note any interventions or techniques used during the session, as well as any homework or assignments given to the client.
5. Discharge Summary Form
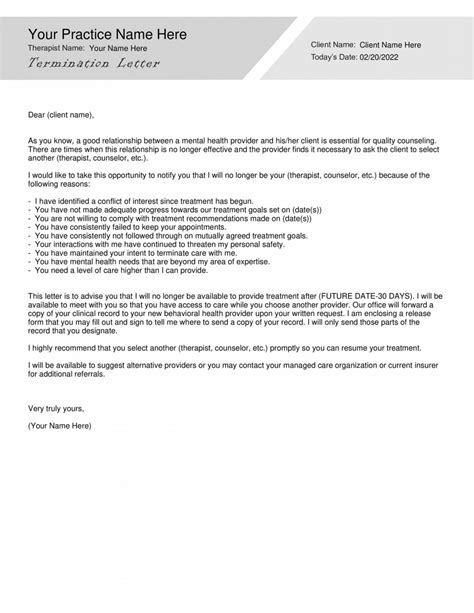
A discharge summary form is used to document the client’s discharge from therapy. This form typically includes information about the client’s treatment outcomes, any remaining symptoms or concerns, and recommendations for future treatment. The form may also include space for the therapist to note any referrals or recommendations for additional services, such as support groups or counseling.
💡 Note: These forms are not exhaustive and may vary depending on the therapist, client, and treatment setting.
Benefits of Using Therapy Forms
Using therapy forms can have several benefits, including: * Improved client outcomes: By using standardized forms, therapists can ensure that they are collecting consistent and accurate information, which can inform treatment decisions and improve client outcomes. * Increased efficiency: Therapy forms can save time and reduce paperwork, allowing therapists to focus on providing high-quality care to their clients. * Enhanced communication: Therapy forms can facilitate communication between therapists, clients, and other healthcare providers, ensuring that everyone is on the same page and working towards the same goals.
Best Practices for Using Therapy Forms
To get the most out of therapy forms, therapists should follow best practices, including: * Using forms consistently and accurately * Ensuring that forms are completed in a timely and thorough manner * Reviewing and updating forms regularly to reflect changes in the client’s treatment plan * Ensuring that forms are stored securely and in accordance with HIPAA regulations
| Form | Purpose |
|---|---|
| Client Intake Form | Gather basic demographic information and mental health history |
| Behavioral Assessment Form | Evaluate client behaviors, thoughts, and feelings |
| Treatment Plan Form | Outline client goals, objectives, and interventions |
| Progress Notes Form | Document client progress and treatment outcomes |
| Discharge Summary Form | Document client discharge and treatment outcomes |
In summary, therapy forms are essential tools used by mental health professionals to assess, diagnose, and treat their clients. By using these forms consistently and accurately, therapists can improve client outcomes, increase efficiency, and enhance communication. By following best practices and using the right forms for the right purposes, therapists can provide high-quality care to their clients and help them achieve their treatment goals.
What is the purpose of a client intake form?
+
The purpose of a client intake form is to gather basic demographic information and mental health history from the client before their first therapy session.
What is a behavioral assessment form used for?
+
A behavioral assessment form is used to evaluate a client’s behaviors, thoughts, and feelings, and to identify any symptoms of mental health conditions.
What is the purpose of a discharge summary form?
+
The purpose of a discharge summary form is to document the client’s discharge from therapy, including their treatment outcomes, any remaining symptoms or concerns, and recommendations for future treatment.