Medicare Paperwork Requirements
Introduction to Medicare Paperwork Requirements

When it comes to Medicare, understanding the paperwork requirements is essential for healthcare providers, patients, and administrators alike. The complexity of Medicare regulations can be overwhelming, but navigating through the necessary documentation is crucial for compliance, reimbursement, and patient care. In this comprehensive guide, we will delve into the world of Medicare paperwork, exploring the various forms, submissions, and record-keeping necessities.
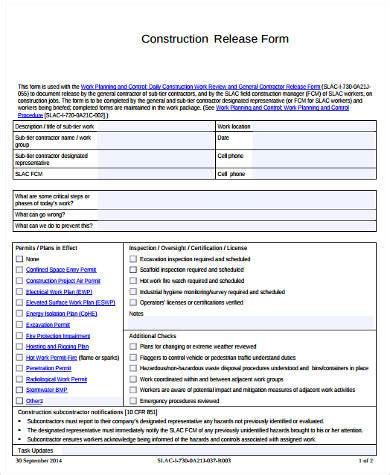
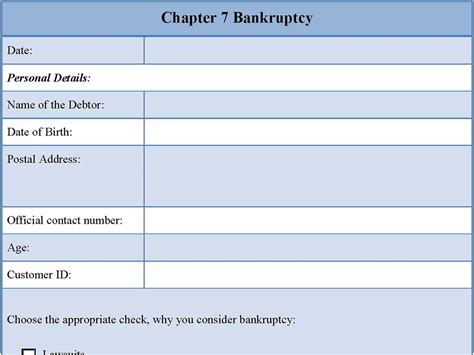
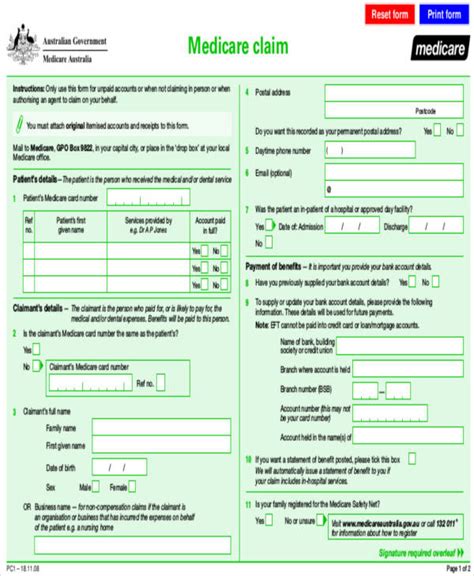
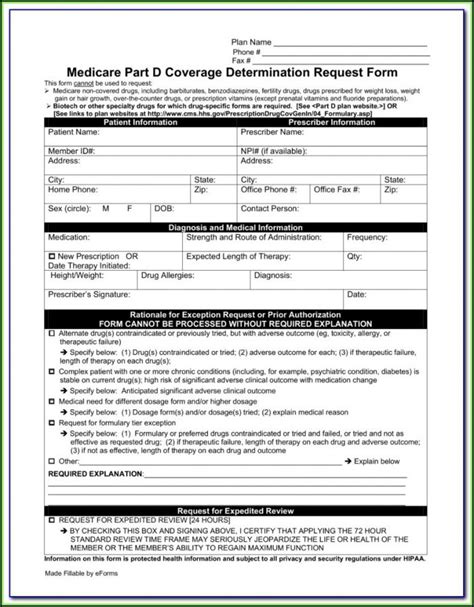
Understanding Medicare Forms and Submissions
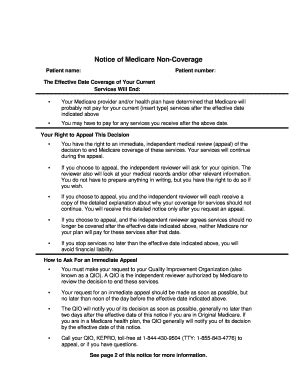
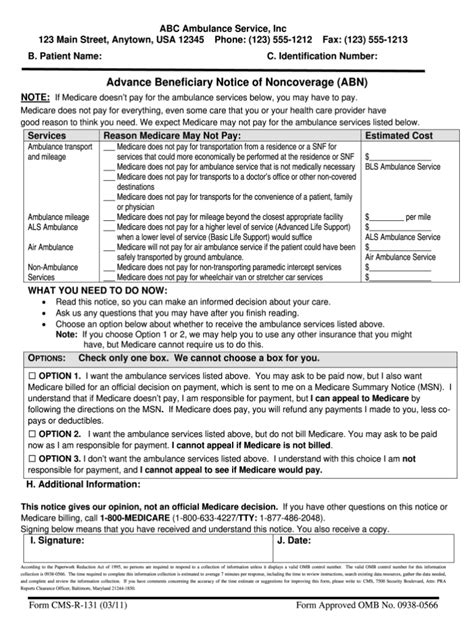
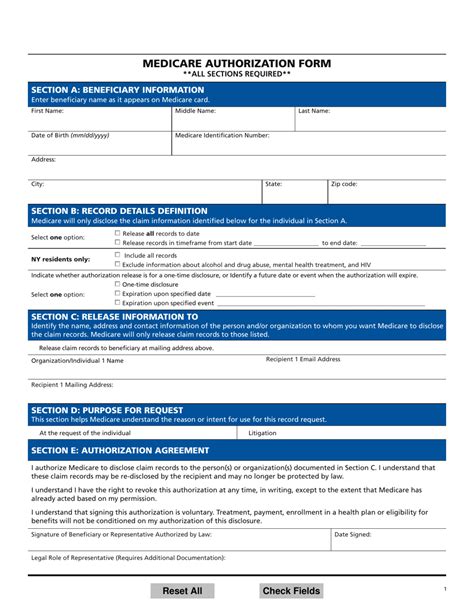
Medicare involves a multitude of forms and submissions that serve different purposes. These include: - CMS-1500: The standard claim form used by healthcare providers to bill Medicare for services rendered. - UB-04: The claim form used by hospitals and other facilities for billing Medicare for inpatient and outpatient services. - ABN (Advance Beneficiary Notice): A notice provided to patients when a service is expected to be denied by Medicare, allowing them to make informed decisions about their care. - HIPAA (Health Insurance Portability and Accountability Act) forms: Essential for protecting patient privacy and ensuring compliance with federal regulations.
These forms are critical for reimbursement, compliance, and maintaining accurate patient records. Understanding when and how to use each form is vital for healthcare providers and administrative staff.
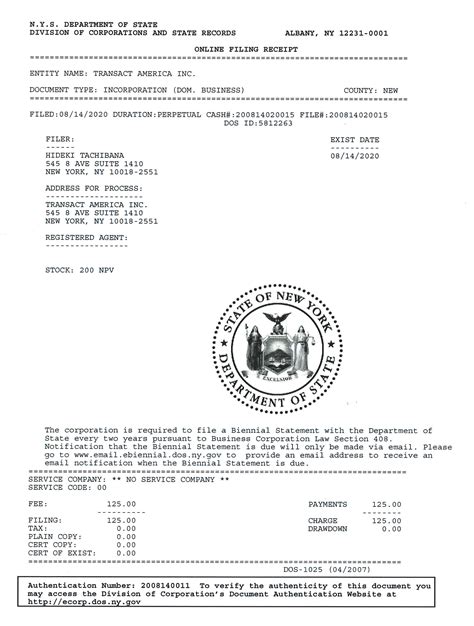
The Importance of Record-Keeping
Accurate and detailed record-keeping is fundamental in Medicare paperwork. Patient records must be maintained securely, with all relevant information documented, including medical history, treatment plans, and correspondence with Medicare. Electronic Health Records (EHRs) have become the standard for managing patient information, offering advantages in terms of accessibility, security, and efficiency. However, whether using physical files or digital systems, the principles of confidentiality, integrity, and availability must be upheld.
Electronic Claims Submission

The transition to electronic claims submission has streamlined the Medicare billing process, reducing errors and increasing the speed of reimbursement. Healthcare providers can submit claims directly to Medicare through approved clearinghouses or directly if they have the necessary infrastructure. This method not only accelerates the payment process but also helps in reducing administrative burdens associated with paper claims.
Compliance and Audits
Medicare compliance is a critical aspect of healthcare administration, with audits serving as a tool to ensure adherence to regulations. Healthcare providers must be prepared to undergo audits, which may involve reviewing patient records, billing practices, and other documentation to verify compliance with Medicare rules. Understanding the audit process and maintaining meticulous records can help providers navigate these situations with confidence.
Technology and Innovations in Medicare Paperwork

The integration of technology in Medicare paperwork has been transformative, offering solutions to long-standing challenges such as inefficiency and inaccuracy. Innovations in electronic health records, billing software, and telehealth platforms are continuously evolving, promising enhanced patient care, streamlined administrative tasks, and better compliance with Medicare regulations.
| Technology | Benefits |
|---|---|
| Electronic Health Records (EHRs) | Improved patient care, enhanced security, and efficiency in record-keeping |
| Billing Software | Streamlined claims submission, reduced errors, and faster reimbursement |
| Telehealth Platforms | Expanded access to care, convenience for patients, and potential for cost savings |
💡 Note: Staying updated with the latest technological advancements and regulatory changes is crucial for navigating the complex landscape of Medicare paperwork efficiently.
Best Practices for Managing Medicare Paperwork
Effective management of Medicare paperwork involves several best practices, including: - Regular Training: Ensuring staff are well-versed in Medicare regulations and paperwork requirements. - Compliance Audits: Conducting internal audits to identify and rectify potential compliance issues. - Patient Education: Informing patients about Medicare benefits, rights, and responsibilities. - Record-Keeping: Maintaining accurate, secure, and accessible patient records.
By adopting these practices, healthcare providers can mitigate risks, ensure compliance, and focus on delivering high-quality patient care.
In wrapping up our exploration of Medicare paperwork requirements, it’s clear that understanding and navigating these complex regulations is vital for healthcare providers, administrators, and patients. By leveraging technology, adhering to best practices, and staying informed about regulatory updates, we can enhance patient care, streamline administrative tasks, and ensure compliance with Medicare regulations. The evolution of Medicare paperwork is ongoing, with innovations and updates continually shaping the landscape. As we move forward, embracing these changes and prioritizing education, compliance, and patient-centered care will be essential for success in the healthcare sector.
What is the primary purpose of the CMS-1500 form in Medicare?
+
The CMS-1500 form is used by healthcare providers to bill Medicare for services rendered. It is a standard claim form that captures essential information about the patient, the services provided, and the charges incurred.
How does electronic claims submission benefit healthcare providers?
+
Electronic claims submission accelerates the reimbursement process, reduces administrative burdens, and minimizes errors compared to traditional paper claims. It also enhances the efficiency and speed of the billing process.
What role does technology play in managing Medicare paperwork?
+
Technology, including electronic health records, billing software, and telehealth platforms, plays a pivotal role in streamlining Medicare paperwork. It improves efficiency, accuracy, and compliance, while also enhancing patient care and access to services.