Hospice Recertification Paperwork Requirements
Introduction to Hospice Recertification
The process of hospice recertification is a critical component of ensuring that patients receive continuous, high-quality care tailored to their needs as their condition progresses. Hospice care is designed for individuals who are terminally ill and have a limited life expectancy, typically six months or less. The recertification process involves periodic assessments and documentation to confirm that the patient still meets the criteria for hospice care. This process is not only essential for maintaining the patient’s eligibility for hospice services but also for ensuring that the care provided is aligned with the patient’s current needs and wishes.
Understanding the Recertification Process
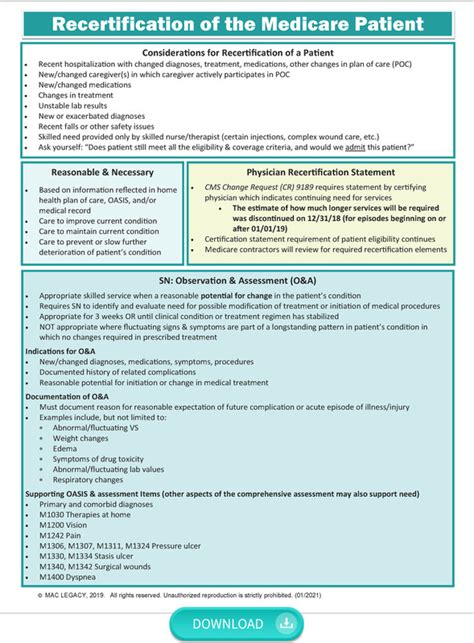
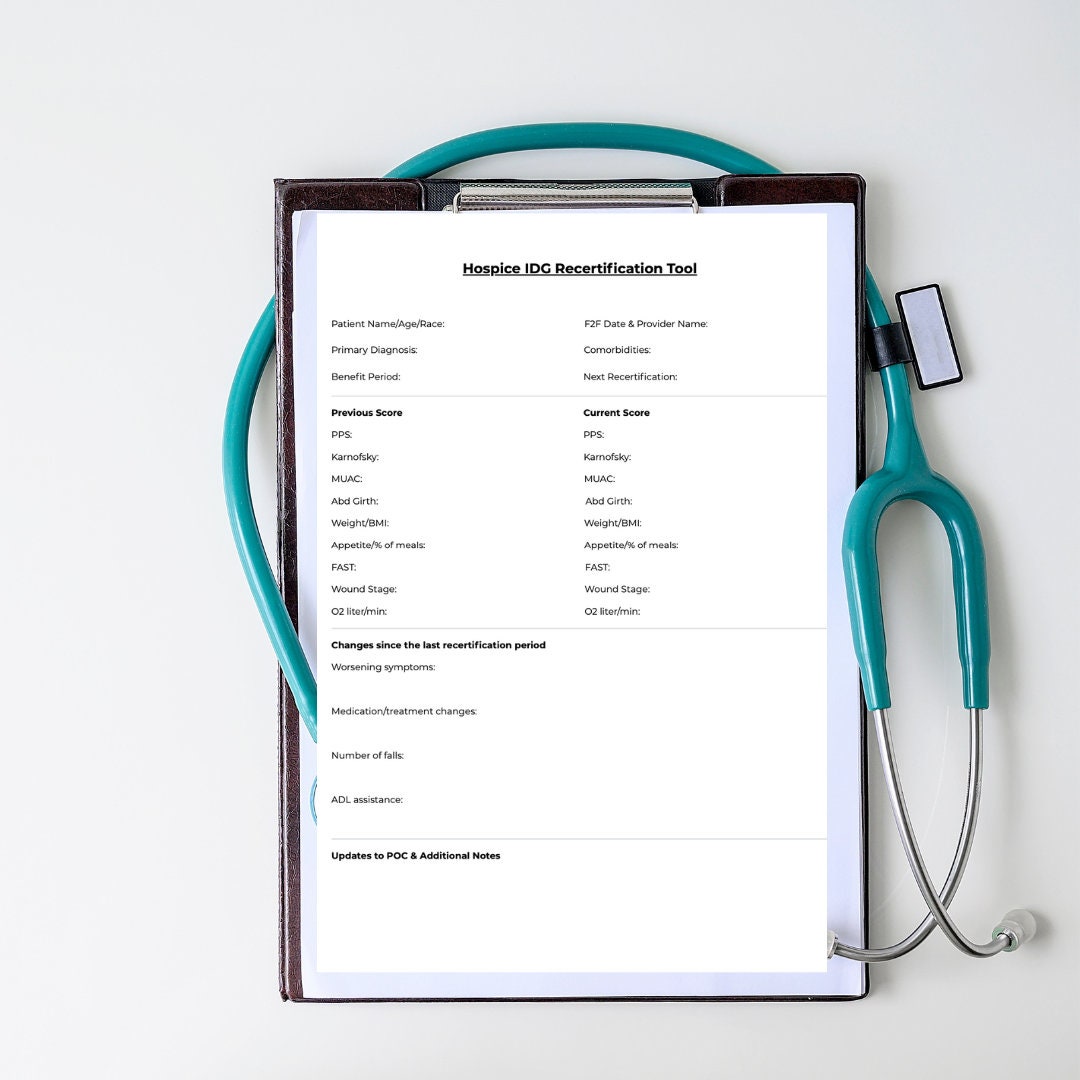
The recertification process for hospice care is governed by regulatory requirements, primarily set forth by the Centers for Medicare and Medicaid Services (CMS) in the United States. These regulations dictate the frequency of recertification, the criteria for eligibility, and the documentation required to support the continuation of hospice care. The process typically involves a comprehensive assessment of the patient’s condition by the hospice team, which includes physicians, nurses, social workers, and other healthcare professionals. This assessment aims to evaluate the patient’s current functional status, symptoms, and overall prognosis to determine if hospice care remains appropriate.
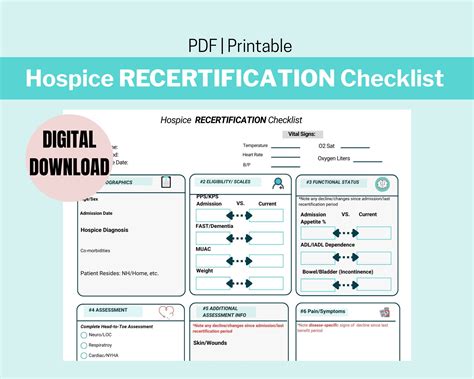
Key Components of Hospice Recertification Paperwork
The paperwork involved in hospice recertification is extensive and must be meticulously completed to ensure that the patient’s care is not interrupted. The key components include: - Initial Certification: Before recertification, an initial certification is required, which involves a physician’s certification that the patient is terminally ill and has a prognosis of six months or less. - Recertification at Intervals: Recertification is required at specific intervals, typically after the initial 90-day period and then at 60-day intervals thereafter, if the patient’s condition persists. - Comprehensive Assessments: Detailed assessments of the patient’s physical, emotional, social, and spiritual needs are conducted at each recertification period. - Care Plans: Individualized care plans are developed or updated based on the assessments, outlining the specific services and interventions the patient will receive. - Physician Certification: A physician must certify that the patient continues to meet the hospice eligibility criteria, including a terminal prognosis and significant decline in functional status.
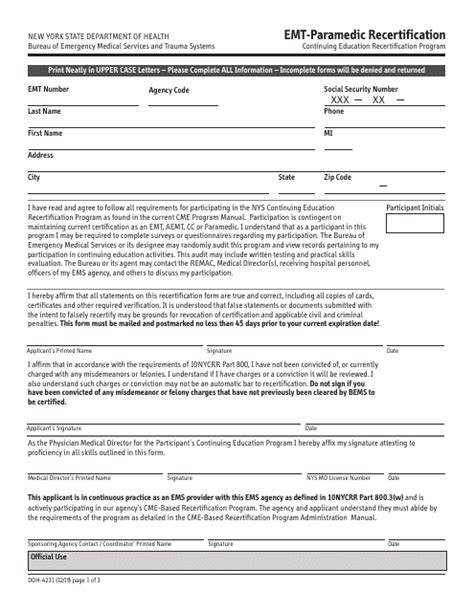
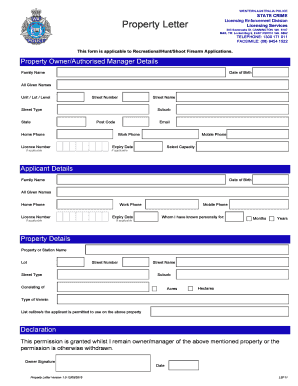
Documentation Requirements
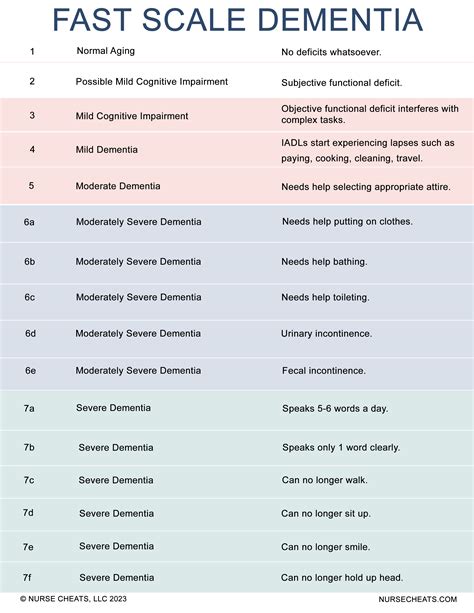
Accurate and comprehensive documentation is crucial for hospice recertification. The required documents typically include: - Medical records detailing the patient’s diagnosis, prognosis, and treatment history. - Certification statements from the patient’s physician confirming the terminal prognosis and the need for hospice care. - Assessment reports from the hospice team outlining the patient’s current condition, symptoms, and care needs. - Care plans and updates to these plans as the patient’s condition changes. - Progress notes from hospice visits and interventions, which help track the patient’s response to care and any changes in their condition.
Importance of Timely Recertification

Timely recertification is essential to avoid gaps in care and to ensure that the patient continues to receive the support and services they need. Delays or failures in recertification can result in interruptions to care, causing undue stress and hardship for the patient and their family. Therefore, hospice providers must prioritize the recertification process, ensuring that all necessary assessments and documentation are completed well in advance of the recertification due date.
Challenges in the Recertification Process
Despite its importance, the recertification process can be challenging. One of the main difficulties is accurately predicting a patient’s life expectancy, as this is inherently uncertain and can vary significantly. Additionally, ensuring that all required documentation is complete, accurate, and submitted on time can be complex, particularly given the interdisciplinary nature of hospice care. Lastly, managing the emotional aspects of recertification, including discussions about prognosis and the continuation of care, requires sensitivity and compassion.
📝 Note: Maintaining clear, detailed records and fostering open communication among the hospice team, the patient, and their family are key strategies for navigating these challenges and ensuring a smooth recertification process.
Conclusion and Future Directions
In summary, hospice recertification is a critical process that ensures patients with terminal illnesses continue to receive appropriate and compassionate care. The process involves regular assessments, detailed documentation, and certification by a physician. While challenges exist, prioritizing clear communication, comprehensive documentation, and a patient-centered approach can help mitigate these issues. As healthcare evolves, it is essential to continue refining the recertification process to better meet the needs of patients and their families, ensuring that hospice care remains a valuable and supportive service for those nearing the end of life.
What is the primary purpose of hospice recertification?
+
The primary purpose of hospice recertification is to confirm that a patient continues to meet the eligibility criteria for hospice care, ensuring they receive appropriate and continuous care tailored to their changing needs.
How often is recertification required for hospice care?
+
Recertification for hospice care is typically required after the initial 90-day period and then at 60-day intervals thereafter, provided the patient’s condition persists and they continue to meet the hospice eligibility criteria.
What are the key components of the recertification paperwork?
+
The key components include initial certification, comprehensive assessments, care plans, physician certification, and detailed documentation of the patient’s condition and care needs.