5 Tips If No Cobra Paperwork

Introduction to COBRA Paperwork
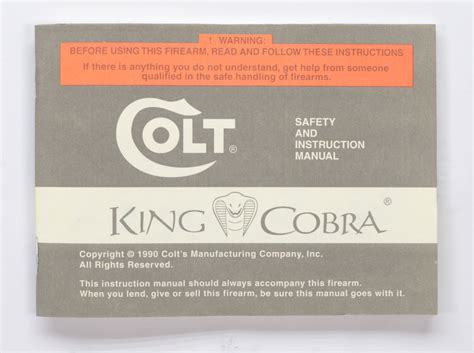
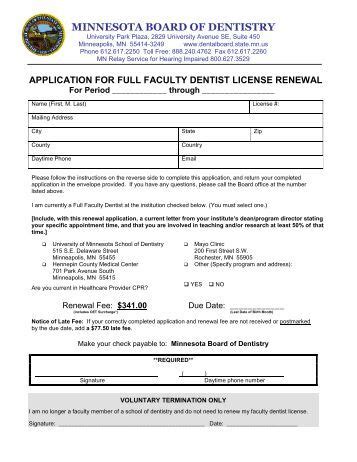
When you leave a job, either voluntarily or involuntarily, and you were covered under your employer’s group health plan, you may be eligible for COBRA (Consolidated Omnibus Budget Reconciliation Act) benefits. COBRA allows you to temporarily continue your health coverage at your own expense. However, to qualify for and utilize these benefits, certain paperwork must be completed and submitted in a timely manner. But what happens if you don’t receive this crucial paperwork? This situation can be stressful and confusing, especially considering the importance of uninterrupted health insurance coverage.
Understanding COBRA and Its Importance

COBRA is a federal law that requires employers with 20 or more employees to offer continuation of health coverage to employees and their families when they experience a qualifying event, such as job loss, divorce, or death. The covered individual then has the option to continue their health insurance coverage for a specified period, typically up to 18 or 36 months, depending on the qualifying event. The importance of COBRA lies in its ability to provide a safety net, ensuring that individuals and families do not experience a gap in health coverage during a time of transition or need.
What to Do If You Don’t Receive COBRA Paperwork
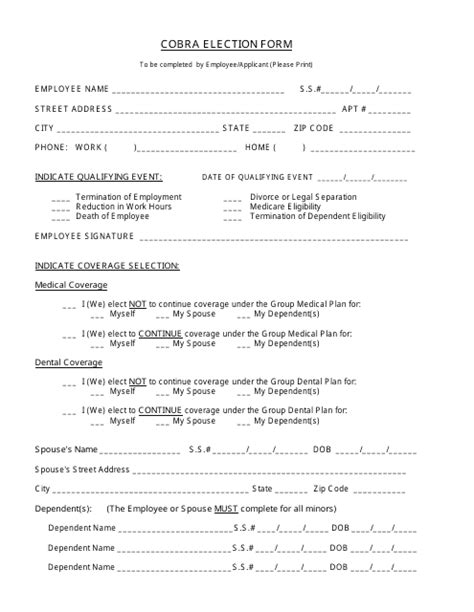
If you are eligible for COBRA benefits but do not receive the necessary paperwork from your employer or the plan administrator, there are several steps you can take: - Contact Your HR Department: Reach out to your former employer’s Human Resources department to inquire about the status of your COBRA paperwork. They can inform you about the process and when you might expect to receive the necessary documents. - Reach Out to the Plan Administrator: If your employer uses an external administrator for their health plan, you may need to contact this entity directly. They can provide information on how to proceed with your COBRA application. - File a Complaint: If you believe your employer or plan administrator is not complying with COBRA regulations, you can file a complaint with the U.S. Department of Labor. They can investigate and take appropriate action to ensure your rights under COBRA are protected. - Explore Other Coverage Options: While waiting for your COBRA paperwork or if you find out you are not eligible, consider other health insurance options such as the Health Insurance Marketplace, Medicaid (if eligible), or short-term health insurance plans. - Keep Records: Document all your attempts to obtain COBRA paperwork, including dates, times, and details of conversations. This can be useful if you need to prove you took timely action to secure your benefits.
Important Considerations
When dealing with COBRA paperwork issues, it’s crucial to act quickly. COBRA benefits must be elected within 60 days of receiving the election notice, and coverage is typically retroactive to the date of the qualifying event. Missing this deadline can result in loss of coverage. Also, be aware that you will be responsible for paying the full premium (plus a 2% administration fee in some cases) for your continued coverage, which can be more expensive than what you paid as an active employee.
Key Points to Remember
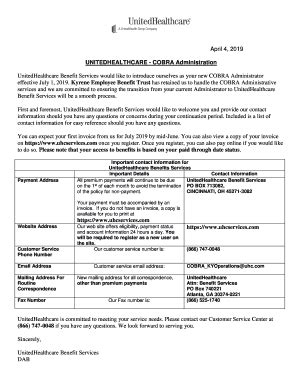
- COBRA provides vital continuation of health insurance coverage for eligible individuals and their families. - Timely receipt and completion of COBRA paperwork are essential to avoid gaps in coverage. - If you encounter issues with receiving COBRA paperwork, proactive steps such as contacting your HR department, plan administrator, or exploring other health insurance options can help mitigate potential problems. - Keeping detailed records of your efforts to secure COBRA benefits can be invaluable in case of disputes or further actions.
📝 Note: Always ensure you understand your specific situation and the options available to you under COBRA, as individual circumstances can affect eligibility and the process for obtaining benefits.
As you navigate the complexities of COBRA and address any issues with receiving the necessary paperwork, staying informed and taking prompt action are key to maintaining uninterrupted health insurance coverage. This not only protects your health and well-being but also shields you from potential financial burdens associated with unforeseen medical expenses.
In summary, understanding your rights and the process under COBRA, coupled with proactive steps to address any issues with paperwork, can provide peace of mind and ensure you and your loved ones maintain access to essential health care services during times of transition.
What is COBRA and how does it work?

+
COBRA is a law that allows eligible employees and their families to continue health coverage at their own expense after a qualifying event, such as job loss. The employer or plan administrator must offer continuation coverage, which the individual can then elect and pay for within a specified timeframe.
How long do I have to elect COBRA benefits after receiving the paperwork?
+
You typically have 60 days from the date you receive the COBRA election notice to decide whether to continue your health coverage under COBRA. It’s crucial to act within this timeframe to avoid losing your eligibility for these benefits.
Can I appeal if my employer denies my COBRA benefits or fails to provide the necessary paperwork?

+
Yes, if you believe your employer or plan administrator has wrongly denied you COBRA benefits or failed to comply with COBRA regulations, you can file a complaint with the U.S. Department of Labor. They will investigate the matter and take appropriate action to enforce COBRA rights.