Paperwork
Cobra Paperwork Deadline

Introduction to Cobra Paperwork Deadline

The COBRA (Consolidated Omnibus Budget Reconciliation Act) paperwork deadline is a crucial aspect of health insurance continuation for individuals who have lost their job or experienced a reduction in work hours. Understanding the deadlines and requirements for COBRA paperwork is essential to ensure uninterrupted health insurance coverage. In this article, we will delve into the world of COBRA paperwork deadlines, exploring the key aspects, benefits, and potential pitfalls.
What is COBRA?
COBRA is a federal law that requires employers with 20 or more employees to offer continuing health insurance coverage to employees who have lost their job or experienced a reduction in work hours. This law applies to most group health plans, including those sponsored by private-sector employers and state and local governments. COBRA coverage is typically available for a period of 18 months, although this can be extended in certain circumstances.
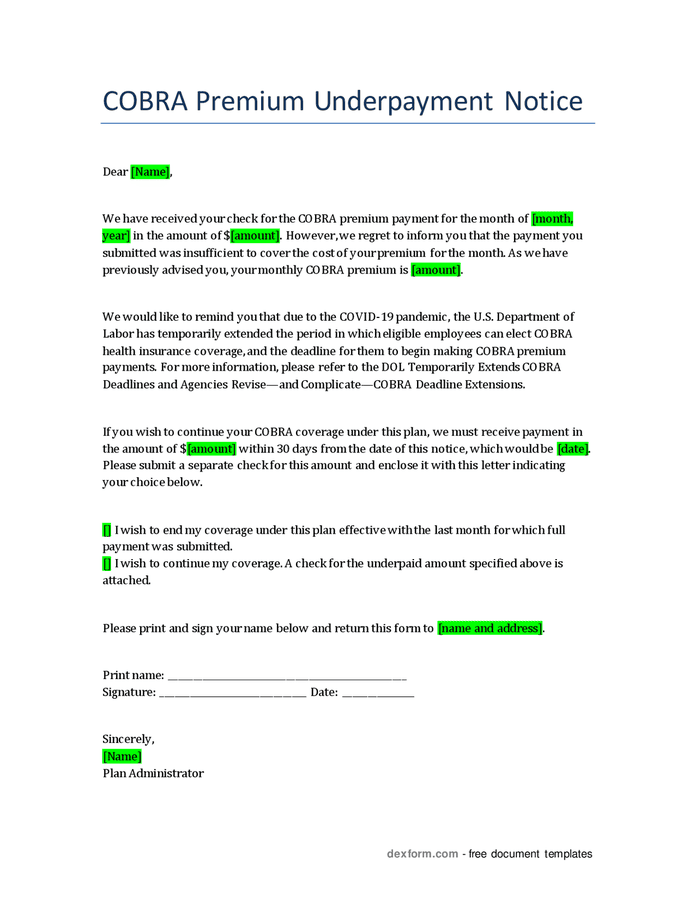
COBRA Paperwork Deadline

The COBRA paperwork deadline is a critical aspect of the continuation coverage process. Generally, the employer has 30 days to notify the plan administrator of a qualifying event, such as an employee’s termination or reduction in work hours. The plan administrator then has 14 days to notify the employee of their COBRA rights and the deadline for electing continuation coverage. The employee typically has 60 days from the date of the qualifying event or the date they receive the COBRA election notice, whichever is later, to elect COBRA coverage.
Key Aspects of COBRA Paperwork Deadline
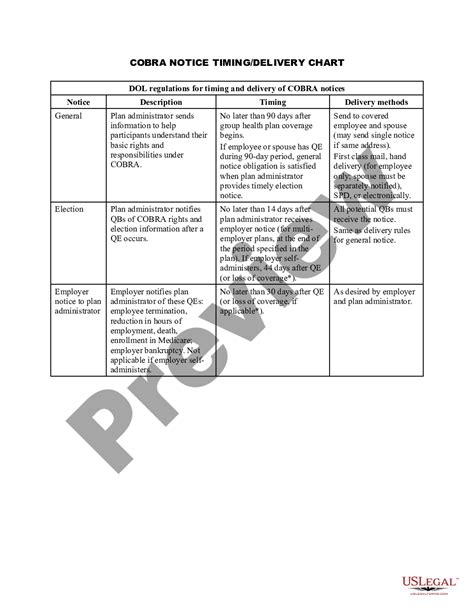
Some key aspects of the COBRA paperwork deadline include: * The employer’s notification to the plan administrator must be made within 30 days of the qualifying event. * The plan administrator’s notification to the employee must be made within 14 days of receiving the employer’s notification. * The employee’s election of COBRA coverage must be made within 60 days of the qualifying event or the date they receive the COBRA election notice. * Failure to meet these deadlines can result in the loss of COBRA coverage.
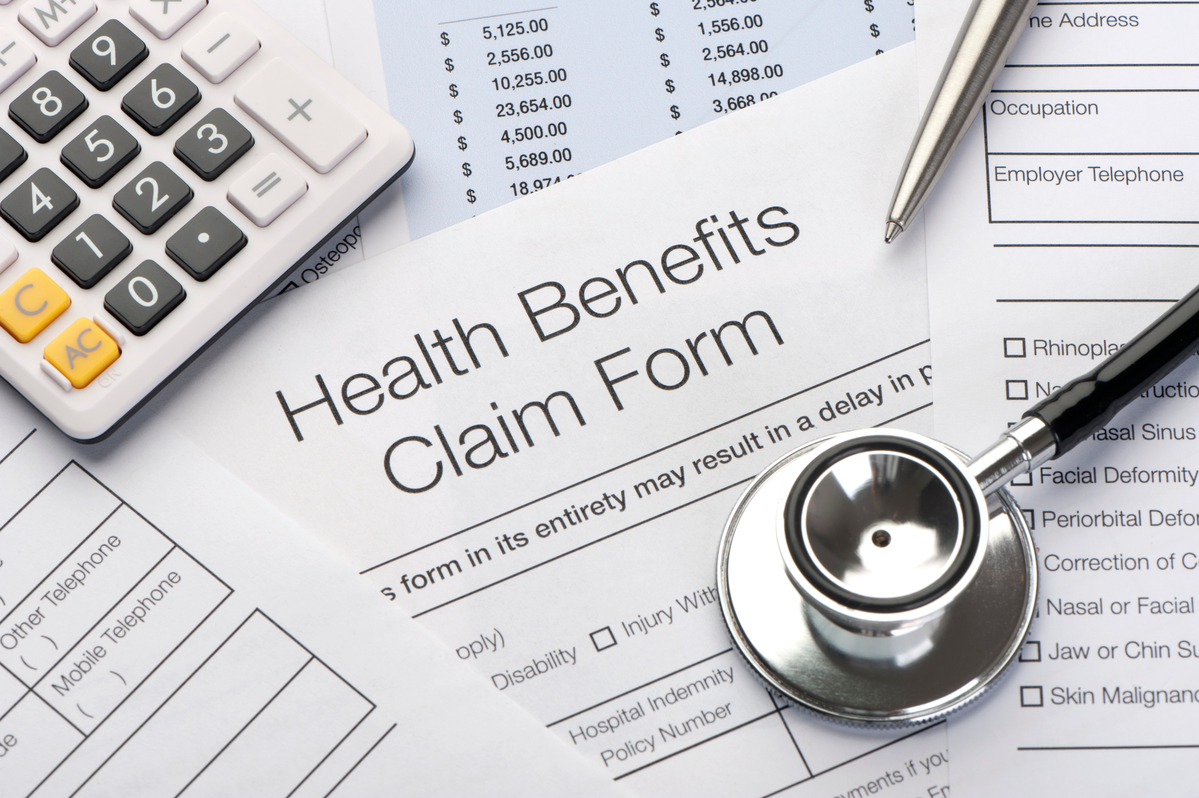
Benefits of COBRA Coverage
COBRA coverage offers several benefits, including: * Continuity of coverage: COBRA allows individuals to maintain their existing health insurance coverage, ensuring uninterrupted protection against medical expenses. * Family coverage: COBRA coverage can be extended to spouses and dependents, providing comprehensive protection for the entire family. * Pre-existing condition coverage: COBRA coverage cannot be denied due to pre-existing conditions, ensuring that individuals with ongoing medical needs can maintain their coverage.
Potential Pitfalls of COBRA Paperwork Deadline
Some potential pitfalls of the COBRA paperwork deadline include: * Missed deadlines: Failing to meet the deadlines for notifying the plan administrator or electing COBRA coverage can result in the loss of continuation coverage. * Incomplete or inaccurate paperwork: Errors or omissions in the COBRA paperwork can delay or deny coverage, highlighting the importance of careful completion and submission of required documents. * Lack of understanding: Failure to comprehend the COBRA paperwork deadline and requirements can lead to confusion, delays, or missed opportunities for continuation coverage.
📝 Note: It is essential to carefully review and understand the COBRA paperwork deadline and requirements to ensure uninterrupted health insurance coverage.
Conclusion and Next Steps

In conclusion, the COBRA paperwork deadline is a critical aspect of health insurance continuation for individuals who have lost their job or experienced a reduction in work hours. Understanding the deadlines and requirements for COBRA paperwork is essential to ensure uninterrupted health insurance coverage. By carefully reviewing and completing the necessary paperwork, individuals can maintain their existing coverage, ensuring comprehensive protection against medical expenses. To summarize, the key points to remember are: * The employer has 30 days to notify the plan administrator of a qualifying event. * The plan administrator has 14 days to notify the employee of their COBRA rights. * The employee has 60 days to elect COBRA coverage. * COBRA coverage offers continuity of coverage, family coverage, and pre-existing condition coverage.
What is the COBRA paperwork deadline for employers?
+
The employer has 30 days to notify the plan administrator of a qualifying event, such as an employee’s termination or reduction in work hours.
How long does the employee have to elect COBRA coverage?

+
The employee typically has 60 days from the date of the qualifying event or the date they receive the COBRA election notice, whichever is later, to elect COBRA coverage.
What are the benefits of COBRA coverage?

+
COBRA coverage offers continuity of coverage, family coverage, and pre-existing condition coverage, ensuring comprehensive protection against medical expenses.