5 Tips Cobra Paperwork
Understanding Cobra Paperwork: A Comprehensive Guide

When dealing with COBRA (Consolidated Omnibus Budget Reconciliation Act) paperwork, it’s essential to have a clear understanding of the process and requirements. COBRA is a federal law that allows certain employees and their families to continue health coverage under an employer’s group health plan after a qualifying event, such as job loss or divorce. In this article, we’ll provide 5 tips to help you navigate COBRA paperwork and ensure a smooth transition.
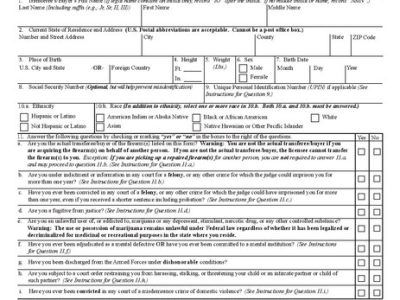
Tip 1: Determine Eligibility
To begin the COBRA process, you must determine if you’re eligible for coverage. Eligibility is typically based on the type of qualifying event and the number of employees in the company. Qualifying events include: * Job loss or reduction in hours * Divorce or separation * Death of the covered employee * Dependent child losing dependent status * Employer bankruptcy It’s crucial to review your company’s health plan and COBRA policy to understand the specific eligibility requirements.
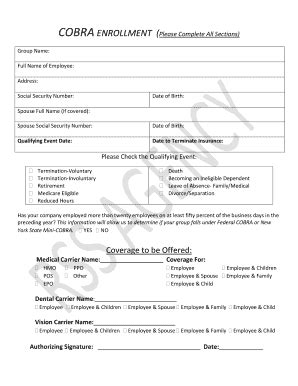
Tip 2: Notify the Administrator
If you’re eligible for COBRA coverage, you must notify the plan administrator within a specified timeframe, usually 60 days. The administrator will provide you with a COBRA election notice, which outlines the details of your coverage, including the premium amount, coverage period, and any other relevant information. Make sure to carefully review the notice and ask questions if you’re unsure about any aspect of the coverage.
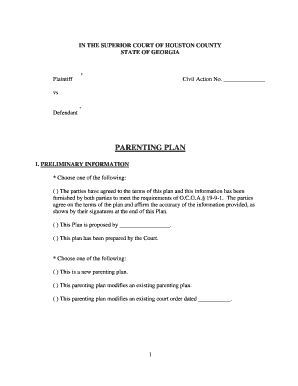
Tip 3: Complete the Election Form

Once you receive the COBRA election notice, you’ll need to complete the election form to choose your coverage options. This form will ask for personal and demographic information, as well as your coverage selections. Be sure to: * Carefully review the form to ensure accuracy * Choose the correct coverage options, including the type of plan and dependents to be covered * Submit the form within the specified timeframe, usually 60 days
Tip 4: Pay Premiums on Time

To maintain COBRA coverage, you must pay premiums on time. Premium payments are typically due on a monthly basis, and late payments may result in termination of coverage. Make sure to: * Set up a payment schedule to ensure timely payments * Keep records of your premium payments * Notify the administrator of any changes to your payment information
Tip 5: Review and Update Coverage

COBRA coverage is typically available for 18-36 months, depending on the qualifying event. During this time, it’s essential to review and update your coverage as needed. Be sure to: * Notify the administrator of any changes to your dependents or coverage needs * Review your coverage options and make changes as necessary * Keep records of your coverage and premium payments
📝 Note: It's essential to keep accurate records of your COBRA paperwork, including premium payments and coverage documents, in case of any discrepancies or disputes.
As you navigate the COBRA paperwork process, remember to stay organized, review your coverage options carefully, and ask questions if you’re unsure about any aspect of the process. By following these 5 tips, you can ensure a smooth transition and maintain essential health coverage during a time of change.
In summary, understanding COBRA paperwork is crucial for maintaining health coverage after a qualifying event. By determining eligibility, notifying the administrator, completing the election form, paying premiums on time, and reviewing and updating coverage, you can navigate the COBRA process with confidence. Whether you’re an employee, employer, or administrator, it’s essential to stay informed and up-to-date on the latest COBRA regulations and requirements.
What is the purpose of COBRA paperwork?
+
The purpose of COBRA paperwork is to provide continued health coverage to employees and their families after a qualifying event, such as job loss or divorce.
How long do I have to notify the administrator of my eligibility?

+
You typically have 60 days to notify the administrator of your eligibility for COBRA coverage.
Can I change my coverage options during the COBRA period?
+