Cobra Paperwork Arrival Time
Understanding the Cobra Paperwork Arrival Time
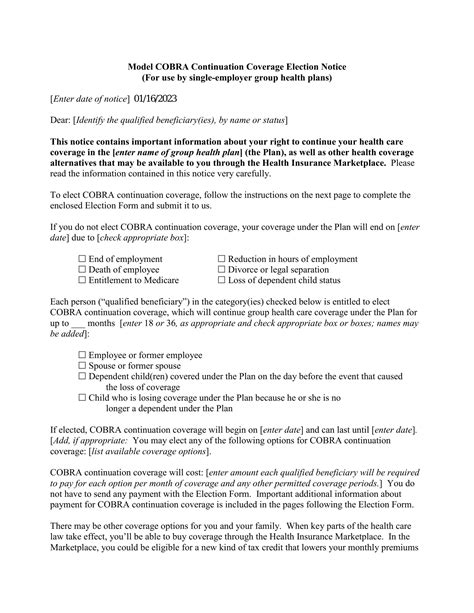
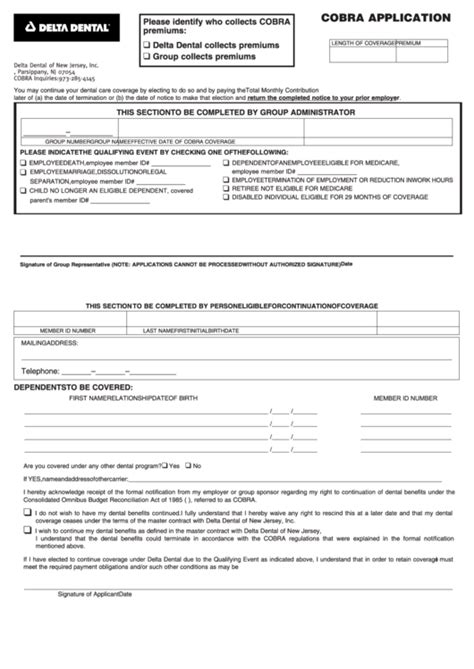
The Cobra paperwork arrival time is a crucial aspect of the Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985. This law requires employers with 20 or more employees to offer continued health coverage to employees and their dependents after a qualifying event, such as job loss, divorce, or death. When an individual experiences a qualifying event, they are eligible to receive COBRA paperwork, which outlines their options for continuing health coverage. The timeframe for receiving this paperwork is essential, as it affects the individual’s ability to make informed decisions about their health insurance.
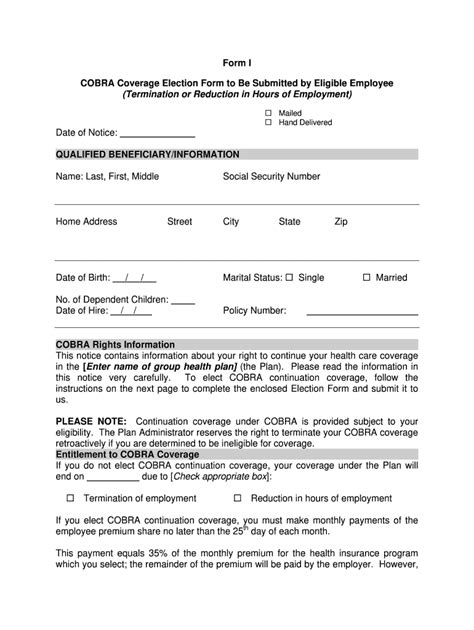
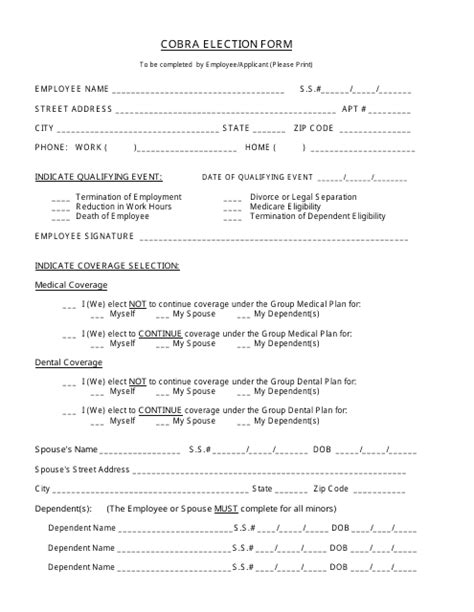
Key Components of Cobra Paperwork

The COBRA paperwork typically includes the following key components: * A description of the qualifying event and the individual’s eligibility for COBRA coverage * The cost of COBRA coverage, which is usually 102% of the employer’s cost for the same coverage * The duration of COBRA coverage, which is typically 18 months for employees and their dependents * The deadline for electing COBRA coverage, which is usually 60 days from the date of the qualifying event * The consequences of not electing COBRA coverage, such as the loss of health insurance and potential gaps in coverage
Timeline for Receiving Cobra Paperwork

The timeline for receiving COBRA paperwork varies depending on the circumstances of the qualifying event. Generally, the employer or plan administrator must provide the COBRA paperwork within the following timeframes: * For qualifying events related to employment, such as job loss or reduction in hours, the COBRA paperwork must be provided within 44 days of the event * For qualifying events related to divorce or legal separation, the COBRA paperwork must be provided within 14 days of the event * For qualifying events related to death or Medicare entitlement, the COBRA paperwork must be provided within 14 days of the event
📝 Note: It is essential to review the COBRA paperwork carefully and understand the options and deadlines for electing coverage. If the paperwork is not received within the specified timeframe, the individual should contact the employer or plan administrator to request the necessary documents.
Consequences of Delayed Cobra Paperwork
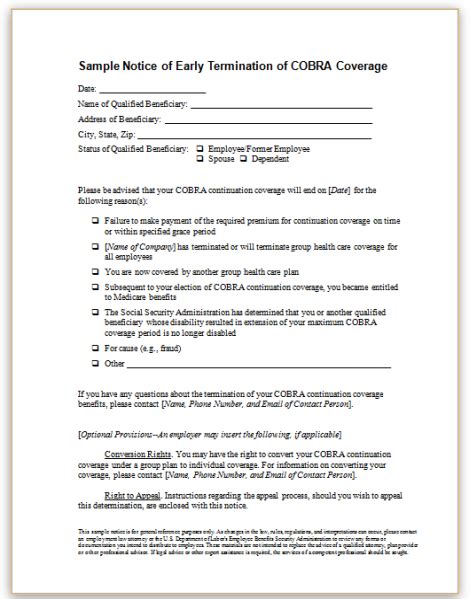
Delayed COBRA paperwork can have significant consequences for individuals who are eligible for continued health coverage. If the paperwork is not received within the specified timeframe, the individual may: * Miss the deadline for electing COBRA coverage, resulting in the loss of health insurance * Experience gaps in coverage, which can lead to financial burdens and health risks * Be required to pay higher premiums or penalties for late enrollment in a new health plan
Best Practices for Employers and Plan Administrators
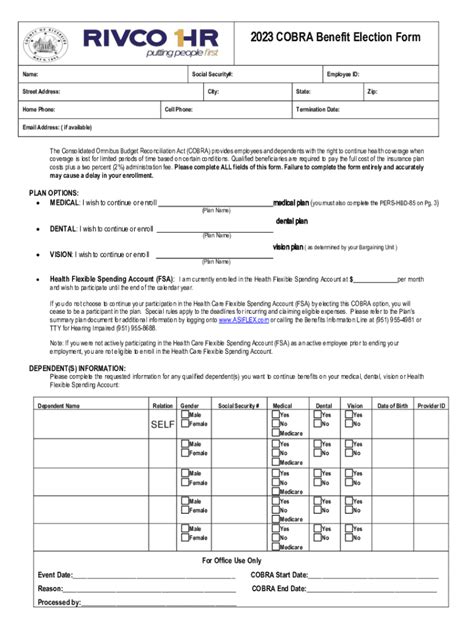
To ensure compliance with COBRA regulations and avoid delays in providing COBRA paperwork, employers and plan administrators should: * Develop a systematic process for tracking qualifying events and generating COBRA paperwork * Designate a responsible individual or department to handle COBRA administration and communication * Provide clear and concise instructions to employees and their dependents regarding COBRA options and deadlines * Maintain accurate records of COBRA elections and coverage, including documentation of qualifying events and notification dates
| Qualifying Event | COBRA Paperwork Deadline |
|---|---|
| Job loss or reduction in hours | 44 days |
| Divorce or legal separation | 14 days |
| Death or Medicare entitlement | 14 days |

In summary, the COBRA paperwork arrival time is a critical aspect of the COBRA process, and individuals who are eligible for continued health coverage must receive the necessary documents within the specified timeframe. Employers and plan administrators must develop systematic processes for tracking qualifying events and generating COBRA paperwork to ensure compliance with COBRA regulations and avoid delays. By understanding the key components of COBRA paperwork and the timeline for receiving these documents, individuals can make informed decisions about their health insurance and avoid gaps in coverage.
What is the purpose of COBRA paperwork?
+
The purpose of COBRA paperwork is to inform individuals of their options for continuing health coverage after a qualifying event, such as job loss or divorce.
How long do I have to elect COBRA coverage?
+
You typically have 60 days from the date of the qualifying event to elect COBRA coverage.
What happens if I miss the deadline for electing COBRA coverage?
+
If you miss the deadline for electing COBRA coverage, you may lose your health insurance and experience gaps in coverage, which can lead to financial burdens and health risks.