Cobra Paperwork Deadline
Understanding the Cobra Paperwork Deadline

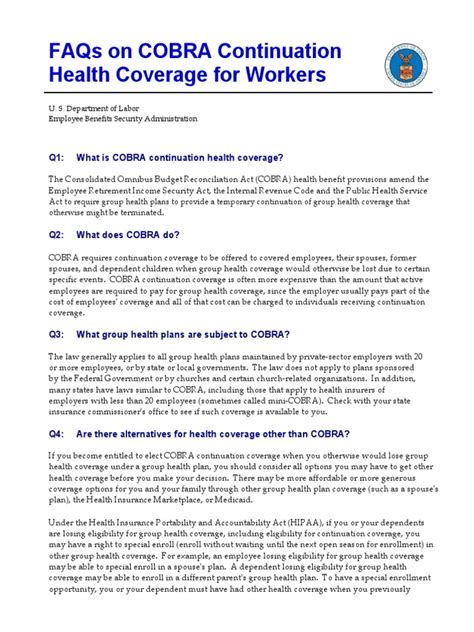
The Cobra paperwork deadline is a critical aspect of the Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985, which provides employees and their families with the opportunity to continue their health insurance coverage after a qualifying event, such as job loss or divorce. This deadline is essential to ensure that individuals can maintain their health insurance without interruption. In this article, we will delve into the details of the Cobra paperwork deadline, its importance, and the steps to follow to meet this deadline.
What is the Cobra Paperwork Deadline?
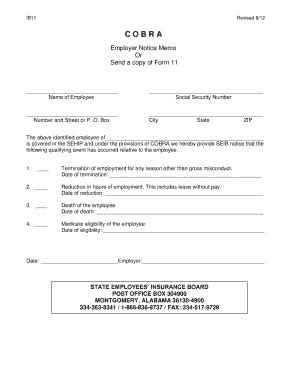
The Cobra paperwork deadline refers to the timeframe within which individuals must submit their application for COBRA coverage after a qualifying event. This deadline is typically 60 days from the date of the qualifying event or the date the individual receives the COBRA election notice, whichever is later. It is crucial to note that this deadline is strictly enforced, and failure to submit the application within the specified timeframe may result in the loss of COBRA eligibility.
Why is the Cobra Paperwork Deadline Important?

The Cobra paperwork deadline is important for several reasons: * Continuity of Coverage: Meeting the deadline ensures that individuals can maintain their health insurance coverage without interruption, which is vital for those with ongoing medical needs. * Avoidance of Gaps in Coverage: Failing to meet the deadline may result in a gap in coverage, leaving individuals and their families without health insurance and exposed to financial risks. * Compliance with Regulations: The Cobra paperwork deadline is a regulatory requirement, and employers and plan administrators must adhere to it to ensure compliance with COBRA regulations.
Steps to Meet the Cobra Paperwork Deadline
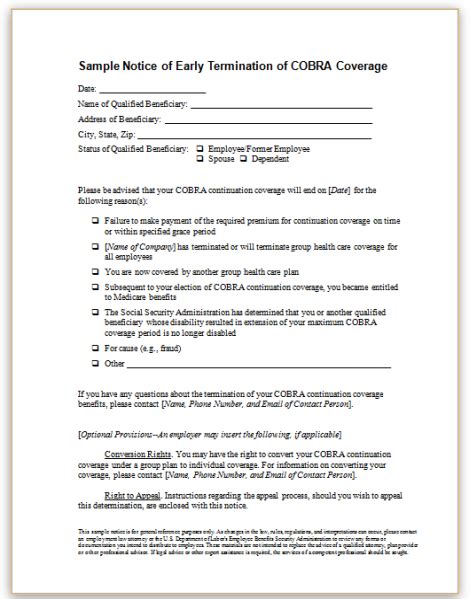
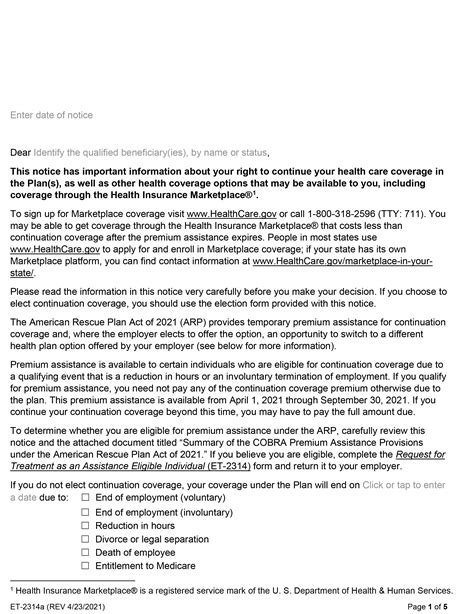
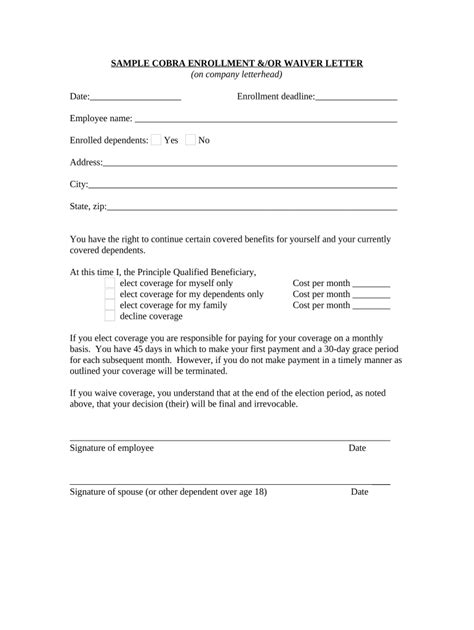
To meet the Cobra paperwork deadline, individuals should follow these steps: * Receive the COBRA Election Notice: After a qualifying event, the employer or plan administrator will provide the individual with a COBRA election notice, which outlines the deadline for submitting the application. * Review the Notice Carefully: Individuals should carefully review the notice to understand the deadline, the cost of coverage, and the procedures for submitting the application. * Gather Required Information: Individuals should gather all required information, including the qualifying event, dependent information, and payment details. * Submit the Application: The individual should submit the application within the specified deadline, ensuring that all required information is complete and accurate. * Make the Initial Payment: After submitting the application, the individual must make the initial payment for COBRA coverage, which is typically due within 45 days of the election.
📝 Note: It is essential to keep a record of the application submission, including the date and time of submission, as well as any subsequent correspondence with the employer or plan administrator.
Consequences of Missing the Cobra Paperwork Deadline
Missing the Cobra paperwork deadline can have significant consequences, including: * Loss of COBRA Eligibility: Failure to submit the application within the deadline may result in the loss of COBRA eligibility, leaving individuals and their families without health insurance. * Gaps in Coverage: A gap in coverage may occur, exposing individuals and their families to financial risks and potential medical expenses. * Delayed Coverage: If the individual is able to submit the application after the deadline, coverage may be delayed, resulting in a gap in coverage.
Best Practices for Meeting the Cobra Paperwork Deadline
To ensure that individuals meet the Cobra paperwork deadline, the following best practices can be followed: * Understand the Deadline: Clearly understand the deadline and the consequences of missing it. * Plan Ahead: Plan ahead and gather all required information before the deadline. * Submit the Application Early: Submit the application well before the deadline to avoid any last-minute issues. * Follow Up: Follow up with the employer or plan administrator to confirm receipt of the application and to address any issues that may arise.
What is the typical Cobra paperwork deadline?
+
The typical Cobra paperwork deadline is 60 days from the date of the qualifying event or the date the individual receives the COBRA election notice, whichever is later.
What happens if I miss the Cobra paperwork deadline?
+
If you miss the Cobra paperwork deadline, you may lose your COBRA eligibility, experience a gap in coverage, or face delayed coverage.
How can I ensure that I meet the Cobra paperwork deadline?
+
To ensure that you meet the Cobra paperwork deadline, understand the deadline, plan ahead, submit the application early, and follow up with the employer or plan administrator.
In summary, the Cobra paperwork deadline is a critical aspect of the COBRA regulations, and meeting this deadline is essential to ensure continuity of health insurance coverage. By understanding the deadline, following the steps to meet it, and adhering to best practices, individuals can maintain their health insurance coverage without interruption and avoid the consequences of missing the deadline. It is crucial to approach this deadline with careful planning and attention to detail to ensure that individuals and their families receive the health insurance coverage they need.