COBRA Paperwork Timeline
Introduction to COBRA Paperwork
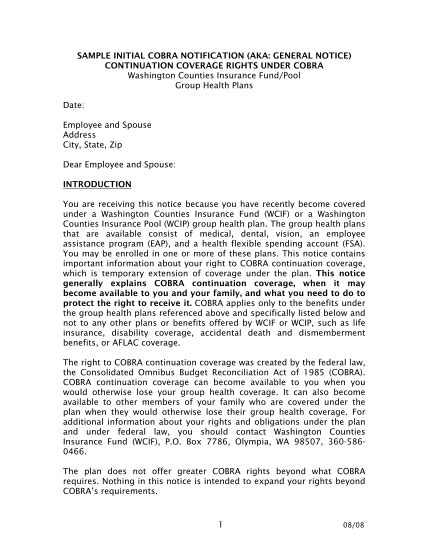
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that allows certain employees and their dependents to continue their health insurance coverage after a qualifying event, such as job loss or divorce. COBRA paperwork is a crucial aspect of this process, as it ensures that eligible individuals receive the necessary information to make informed decisions about their health insurance coverage. In this article, we will discuss the COBRA paperwork timeline and provide a comprehensive guide on how to navigate this complex process.
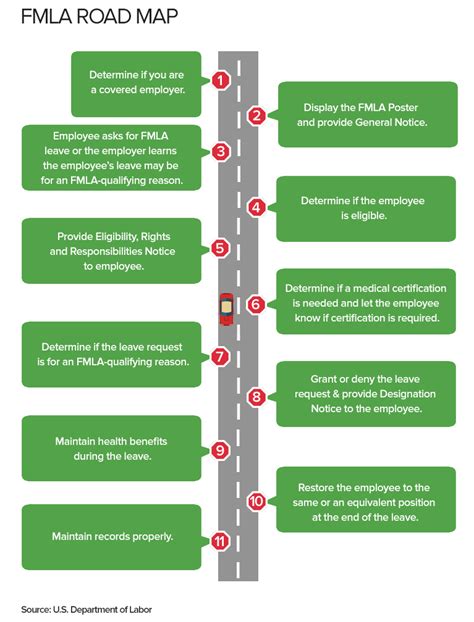
Qualifying Events and Initial Notices
The COBRA paperwork timeline begins with a qualifying event, which can include job loss, reduction in work hours, divorce, death of the covered employee, or a child losing dependent status. Within 30 days of the qualifying event, the employer or plan administrator must provide the employee and their dependents with an initial notice, also known as the COBRA General Notice. This notice explains the COBRA rights and obligations, including the option to continue health insurance coverage and the costs associated with it.
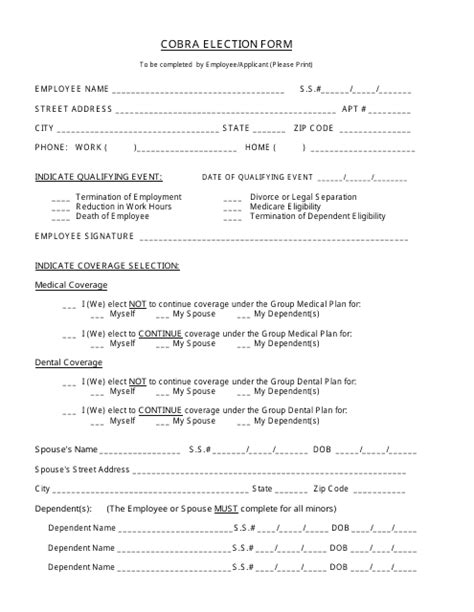
Election Notice and Payment
After the initial notice, the employer or plan administrator must provide an Election Notice to the qualified beneficiaries within 14 days of the qualifying event. The Election Notice outlines the COBRA coverage options, costs, and payment instructions. The qualified beneficiaries then have 60 days to elect COBRA coverage and make the initial payment. The payment must be made within 45 days of the election, and subsequent payments are due on a monthly basis.
COBRA Coverage Period
The COBRA coverage period typically lasts for 18 months from the date of the qualifying event, although it can be extended to 29 months in certain circumstances, such as disability. During this period, the qualified beneficiaries are responsible for paying the full premium, including any administrative fees. The employer or plan administrator must provide coverage notices to the qualified beneficiaries, which outline the terms and conditions of the COBRA coverage.
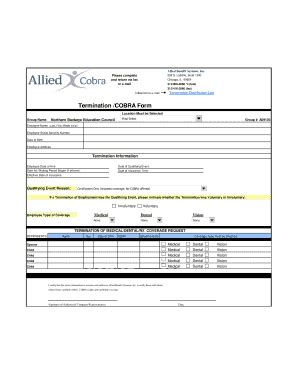
Termination of COBRA Coverage

COBRA coverage can be terminated for various reasons, including failure to pay premiums, eligibility for other group health plan coverage, or entitlement to Medicare. The employer or plan administrator must provide a termination notice to the qualified beneficiaries, which explains the reason for termination and the effective date. The qualified beneficiaries may be eligible for a special enrollment period in another group health plan or individual health insurance coverage.
| Event | Timeline |
|---|---|
| Qualifying Event | Day 1 |
| Initial Notice (COBRA General Notice) | Within 30 days |
| Election Notice | Within 14 days |
| COBRA Election and Payment | Within 60 days and 45 days, respectively |
| COBRA Coverage Period | 18 months (or 29 months in certain circumstances) |
| Termination of COBRA Coverage | Varies depending on reason for termination |
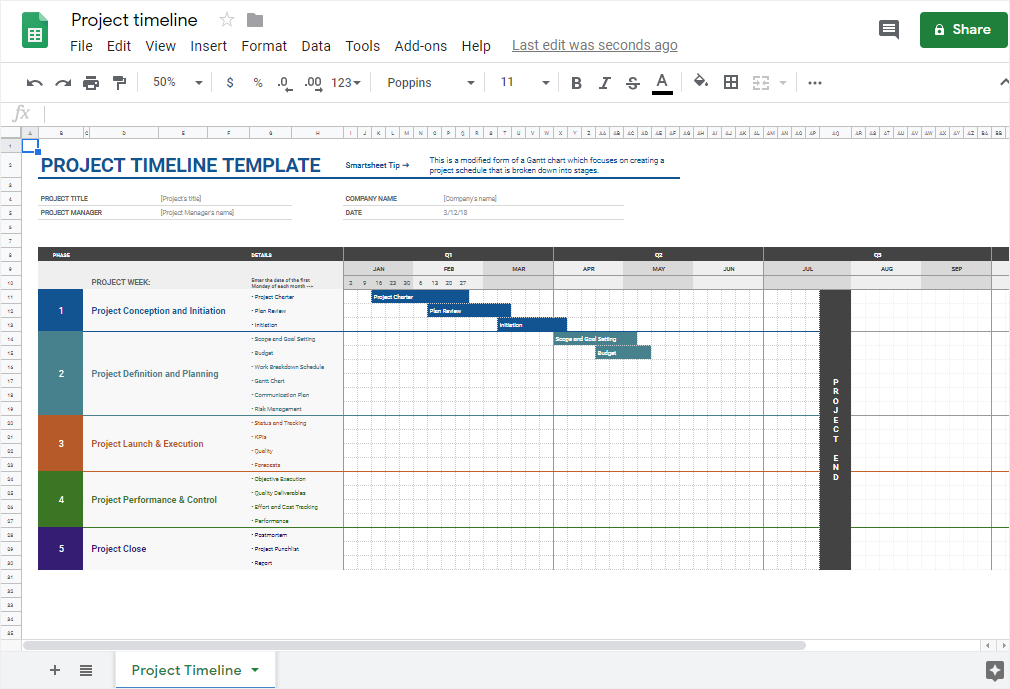
📝 Note: Employers and plan administrators must maintain accurate records of COBRA notices and elections, as failure to comply with COBRA regulations can result in penalties and lawsuits.
To ensure compliance with COBRA regulations, employers and plan administrators should: * Provide timely and accurate notices to qualified beneficiaries * Maintain detailed records of COBRA elections and payments * Offer COBRA coverage options that meet the requirements of the law * Terminate COBRA coverage only for valid reasons and provide proper notice
In summary, the COBRA paperwork timeline is a complex process that requires careful attention to detail and compliance with federal regulations. By understanding the key events and timelines, employers and plan administrators can ensure that qualified beneficiaries receive the necessary information to make informed decisions about their health insurance coverage.
The key points to take away from this article are the importance of timely and accurate notices, the need for detailed record-keeping, and the requirement to offer COBRA coverage options that meet the requirements of the law. By following these guidelines, employers and plan administrators can navigate the COBRA paperwork timeline with confidence and ensure compliance with federal regulations.
What is the purpose of the COBRA General Notice?
+
The COBRA General Notice explains the COBRA rights and obligations, including the option to continue health insurance coverage and the costs associated with it.
How long do qualified beneficiaries have to elect COBRA coverage?

+
Qualified beneficiaries have 60 days to elect COBRA coverage and make the initial payment.
What are the consequences of failing to comply with COBRA regulations?
+
Failure to comply with COBRA regulations can result in penalties and lawsuits.