Fixing UB Insurance Paperwork Issues
Understanding the Complexity of UB Insurance Paperwork
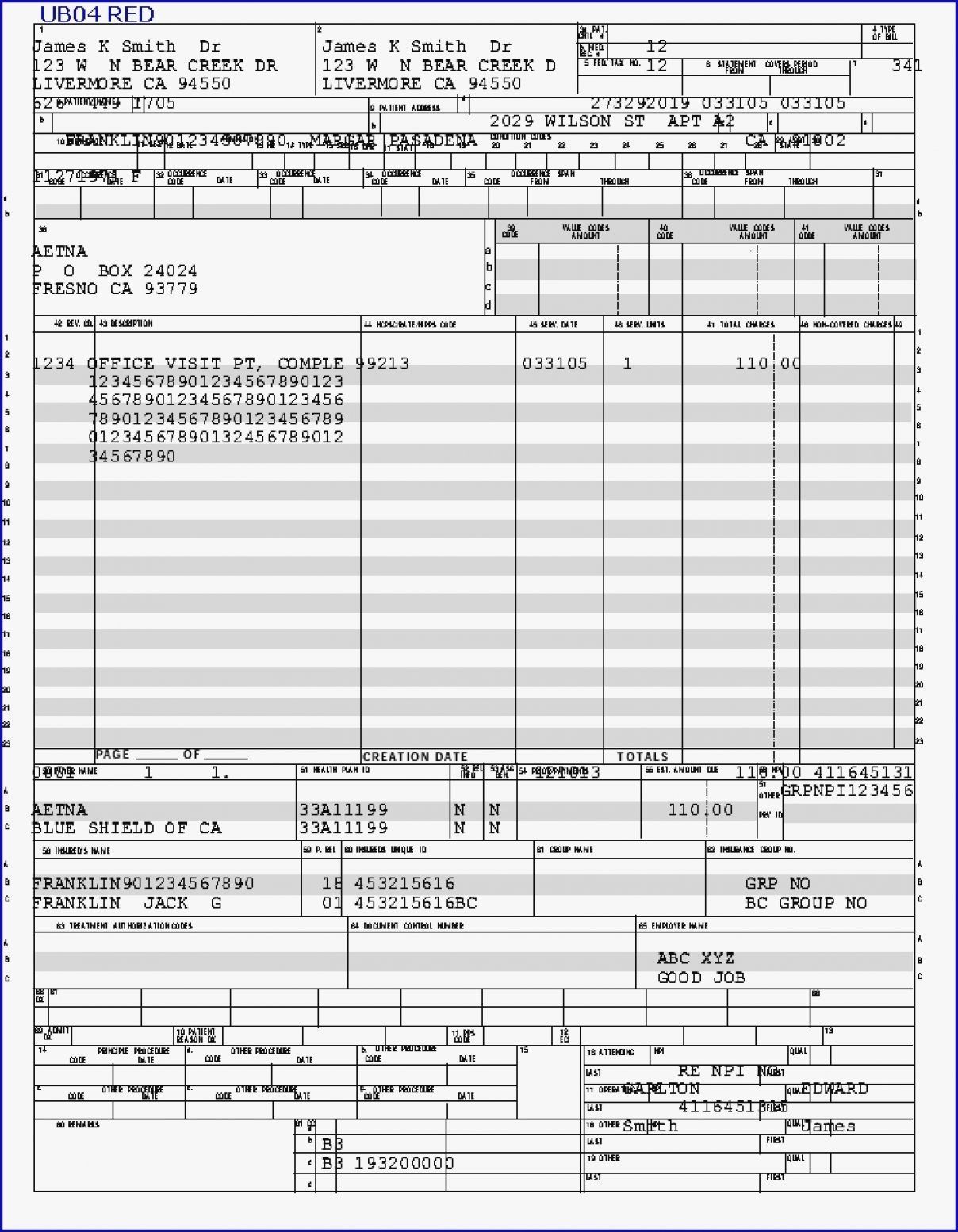
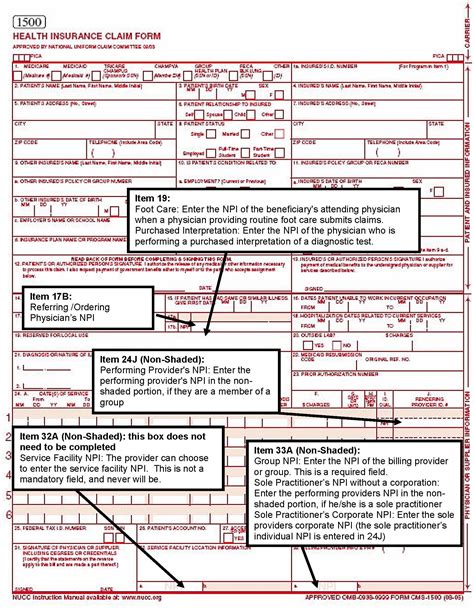
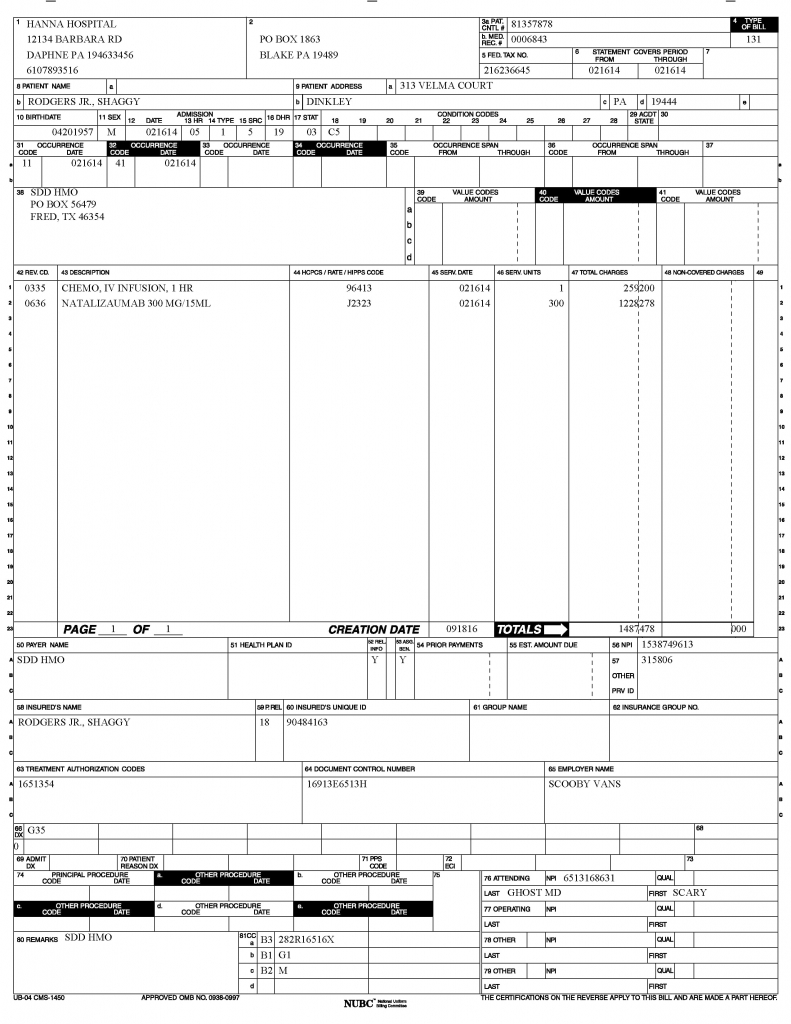
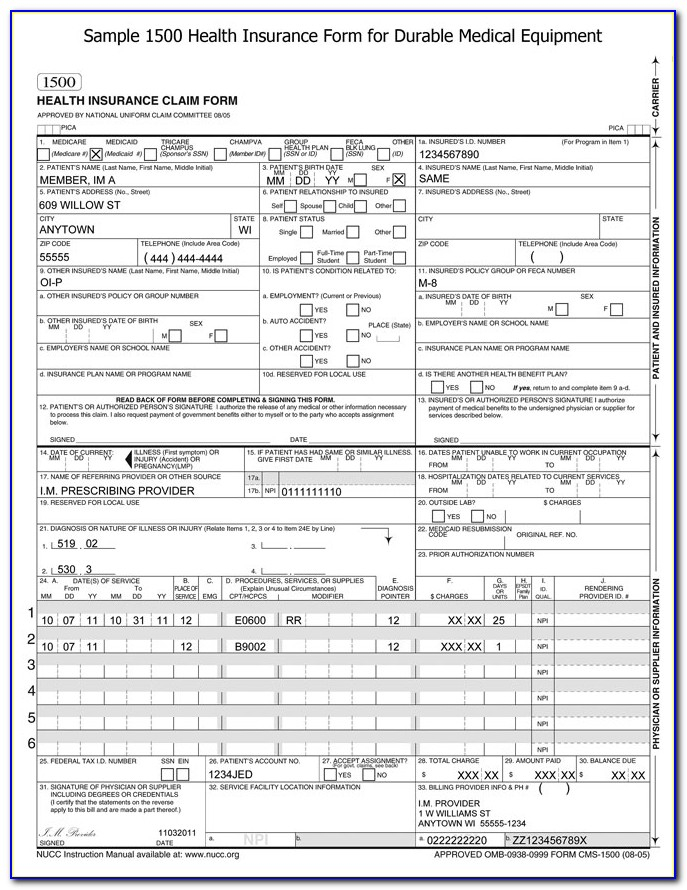
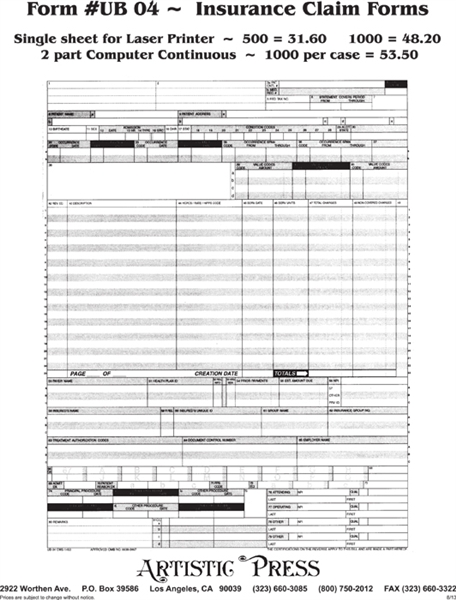
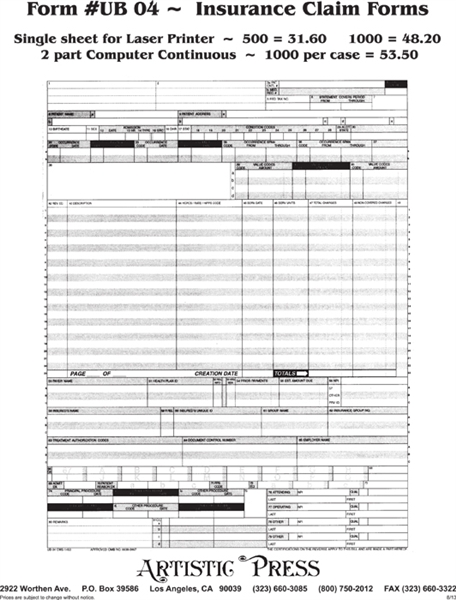
The world of insurance, particularly in the context of healthcare, is filled with complexities and intricacies that can often lead to confusion and frustration for both providers and patients. One of the most critical aspects of healthcare insurance is the paperwork involved, specifically the Uniform Billing (UB) forms. These forms are essential for healthcare providers to submit claims to insurance companies for reimbursement. However, issues with UB insurance paperwork can arise, causing delays, denials, and a significant amount of administrative hassle. In this article, we will delve into the common issues associated with UB insurance paperwork and explore strategies for resolving these problems efficiently.
Common Issues with UB Insurance Paperwork
Several issues can plague the UB insurance paperwork process, including:
- Inaccurate or Missing Information: One of the most common problems is the inclusion of incorrect or incomplete patient and insurance information. This can lead to claims being denied or delayed.
- Incorrect Coding: The use of incorrect diagnosis or procedure codes can result in claims being rejected. Staying up-to-date with coding changes and ensuring accuracy is crucial.
- Insufficient Documentation: Failure to provide adequate supporting documentation can lead to claims being denied. This includes medical records, test results, and other relevant information.
- Timeliness: Submitting claims outside the designated timeframe can result in denials. Understanding the filing deadlines and adhering to them is essential.
Strategies for Resolving UB Insurance Paperwork Issues
To mitigate the problems associated with UB insurance paperwork, several strategies can be employed:
- Automated Claim Submission Systems: Utilizing electronic health records (EHRs) and automated claim submission systems can reduce errors and improve the efficiency of the claims process.
- Staff Training: Ensuring that staff members are well-trained in handling UB paperwork, including coding, billing, and claims submission, is vital. Regular updates and workshops can help keep staff informed about changes and best practices.
- Pre-submission Review: Implementing a thorough review process before submitting claims can help identify and correct errors, reducing the likelihood of denials.
- Patient Engagement: Keeping patients informed about their insurance coverage and the claims process can help manage expectations and reduce misunderstandings.
The Role of Technology in Simplifying UB Insurance Paperwork
Technology plays a crucial role in streamlining the UB insurance paperwork process. Electronic claims submission, for example, reduces the time and effort required to process claims, minimizing the potential for human error. Additionally, software solutions can help with coding, billing, and tracking claims, providing real-time updates and facilitating communication between healthcare providers and insurance companies.
| Technology Solution | Benefits |
|---|---|
| Electronic Health Records (EHRs) | Improved accuracy, reduced paperwork, enhanced patient care |
| Automated Claims Submission Systems | Faster claims processing, reduced errors, improved reimbursement rates |
| Coding and Billing Software | Increased coding accuracy, streamlined billing process, reduced denials |
Best Practices for Managing UB Insurance Paperwork
Adopting best practices can help healthcare providers effectively manage UB insurance paperwork and minimize issues. These include:
- Regular Audits: Conducting regular audits of claims and billing processes can help identify areas for improvement and ensure compliance with regulations.
- Clear Communication: Maintaining open and clear communication with patients, staff, and insurance companies is essential for resolving issues promptly and efficiently.
- Continuous Education: Providing ongoing education and training for staff on coding, billing, and insurance regulations can help reduce errors and improve the claims process.
📝 Note: Regularly reviewing and updating billing and coding practices in accordance with the latest regulations and guidelines is crucial for avoiding compliance issues and ensuring smooth reimbursement processes.
In the end, managing UB insurance paperwork effectively is crucial for the financial stability and operational efficiency of healthcare providers. By understanding the common issues, employing strategic solutions, leveraging technology, and adopting best practices, healthcare organizations can navigate the complexities of UB insurance paperwork, ensuring timely and accurate reimbursement for the services they provide. This not only benefits the healthcare providers but also contributes to better patient care and outcomes, which is the ultimate goal of the healthcare system.